Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) can lead to a range of pulmonary complications, including Pulmonary Arterial Hypertension (PAH), which affects between 0.5% and 17.5% of SLE patients. Multiple retrospective studies have indicated that PAH is an independent risk factor for mortality in SLE patients. This study aims to characterize SLE with and without PAH in United States adult population, in-hospital mortality and estimate the impact of PAH in SLE on utilization of healthcare resources.
Methods: We performed a retrospective review of SLE with and without PAH using the National Inpatient Sample (NIS) from 2016 – 2020. We studied the demographic and epidemiological differences as well as mortality outcomes. Healthcare burden was estimated by total hospital charge (THC) and length of stay (LOS). Statistical analysis was performed on STATA, with linear and logistic regression analyses.
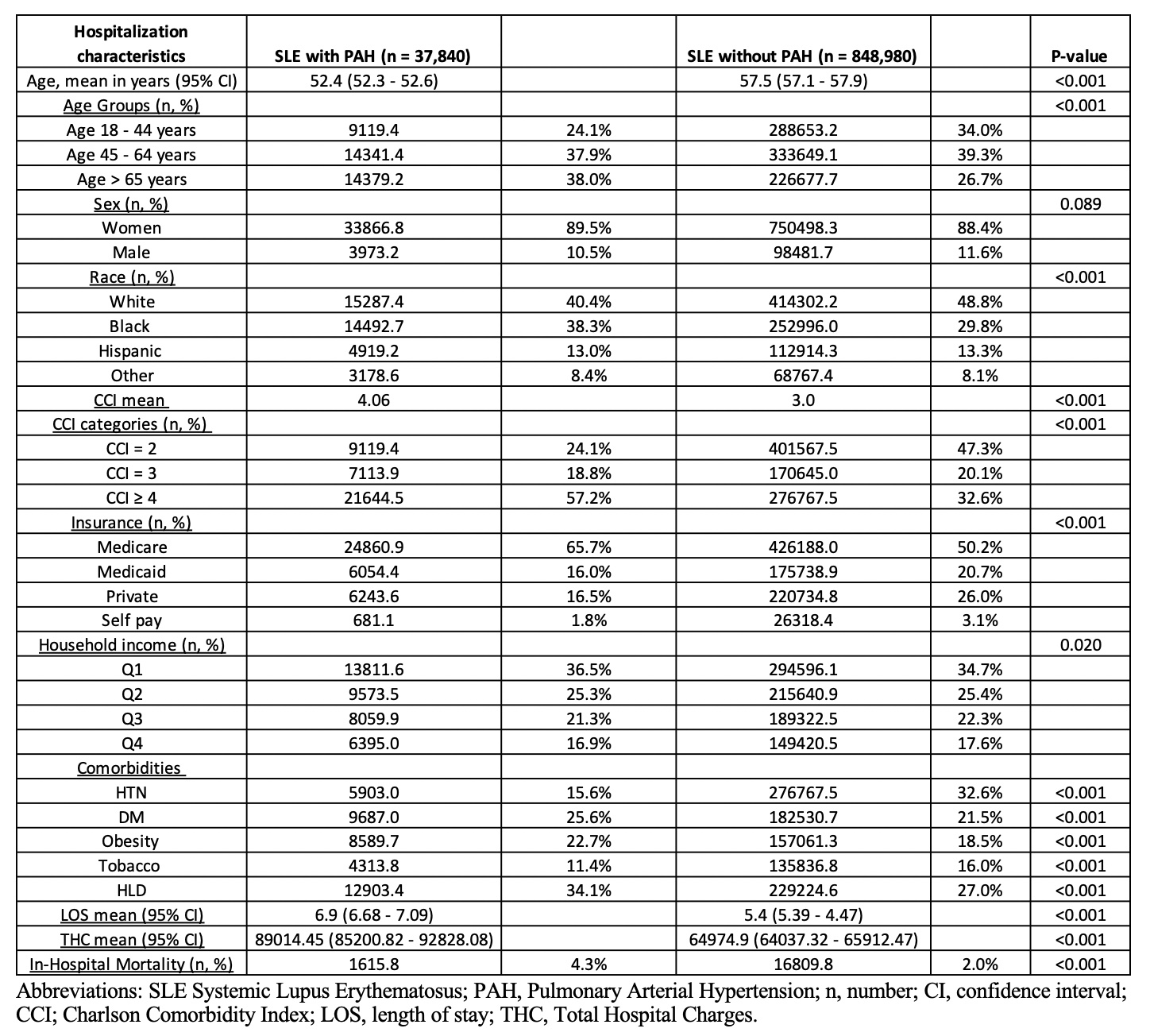
Results: Out of 886,820 adult SLE hospitalizations between 2016 and 2020, 37,840 (4.27%) had concurrent PAH. PAH was associated with high odds ratio (OR) in SLE (OR 2.2, CI 2.14 – 2.26, p< 0.001). SLE-PAH patients had a lower mean age 52.4 vs 57.5 years for SLE without PAH (p< 0.001). There was no statistically significant difference in gender distribution between the two groups. SLE-PAH group had a higher percentage of black patients 38.3% vs 29.8% and a lower percentage of white 40.4% vs 48.8% (p< 0.001). The Charleson comorbidity index (CCI) was higher in SLE-PAH with a mean of 4.06 vs 3 (P value < 0.001). SLE-PAH group had 57.2% patients with CCI ≥ 4 vs 32.6%. There was a statistically significant difference in insurance status between SLE-PAH and SLE without PAH. SLE-PAH had a higher percentage of Medicare 65.7% vs 50.2% and a lower percentage of Medicaid 16% vs 20.7% and private insurance 16.5% vs 26% (p< 0.001). SLE-PAH group had more diabetes (25.6% vs 21.5%), obesity (22.7% vs 18.5%) and hyperlipidemia (34.1% vs 27%), but less systemic hypertension (15.6% vs 32.6%) and less smoking (11.4% vs 16%) all with p< 0.001. The mean LOS in days was higher in SLE-PAH 6.9 (6.68 – 7.09) vs 5.4 (5.39 – 4.47) with p< 0.001. THC in USD was also higher in the study group 89,014.45 vs 64,974.9 (p< 0.001). In-hospital mortality was more than two times higher in SLE-PAH group 4.3% vs 2% with p< 0.001. (Table 1) PAH was associated with higher odds ratio for mortality in SLE patients (OR 1.64, CI 1.45 – 1.87, p< 0.001).
Conclusion: In our analysis, in-patient SLE with PAH group were younger, had more black patients, higher CCI, and more patients with Medicare. The study group also had higher percentage of diabetes and obesity, but lower of systemic hypertension and smoking. LOS and THC were significantly higher in SLE-PAH as well. In-hospital mortality was more than two times higher in SLE-PAH group. SLE-PAH patients had higher odds of in-patient mortality (OR 1.64).
To cite this abstract in AMA style:
Romero Noboa M, Razok A, El Sharu H, Litvin R. Pulmonary Arterial Hypertension in Systemic Lupus Erythematosus: National Inpatient Sample Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pulmonary-arterial-hypertension-in-systemic-lupus-erythematosus-national-inpatient-sample-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pulmonary-arterial-hypertension-in-systemic-lupus-erythematosus-national-inpatient-sample-analysis/