Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Despite significant advances in psoriatic disease (PsD) therapeutics, treatment response remains suboptimal. Even in patients with psoriatic arthritis (PSA) that achieve seemingly controlled inflammation, up to half continue to experience residual symptoms, notably pain and fatigue, which can prevent meaningful improvement in symptoms and quality of life. However, the pathophysiology and effectors of residual pain are not well understood. Functional brain MRI (fMRI) can be used to identify alterations in brain connectivity as a possible basis for residual pain and have the potential to discern inflammatory driven pain from centrally-provoked pain. Here we describe pilot fMRI data showing neuroconnectivity changes in those with PsD.
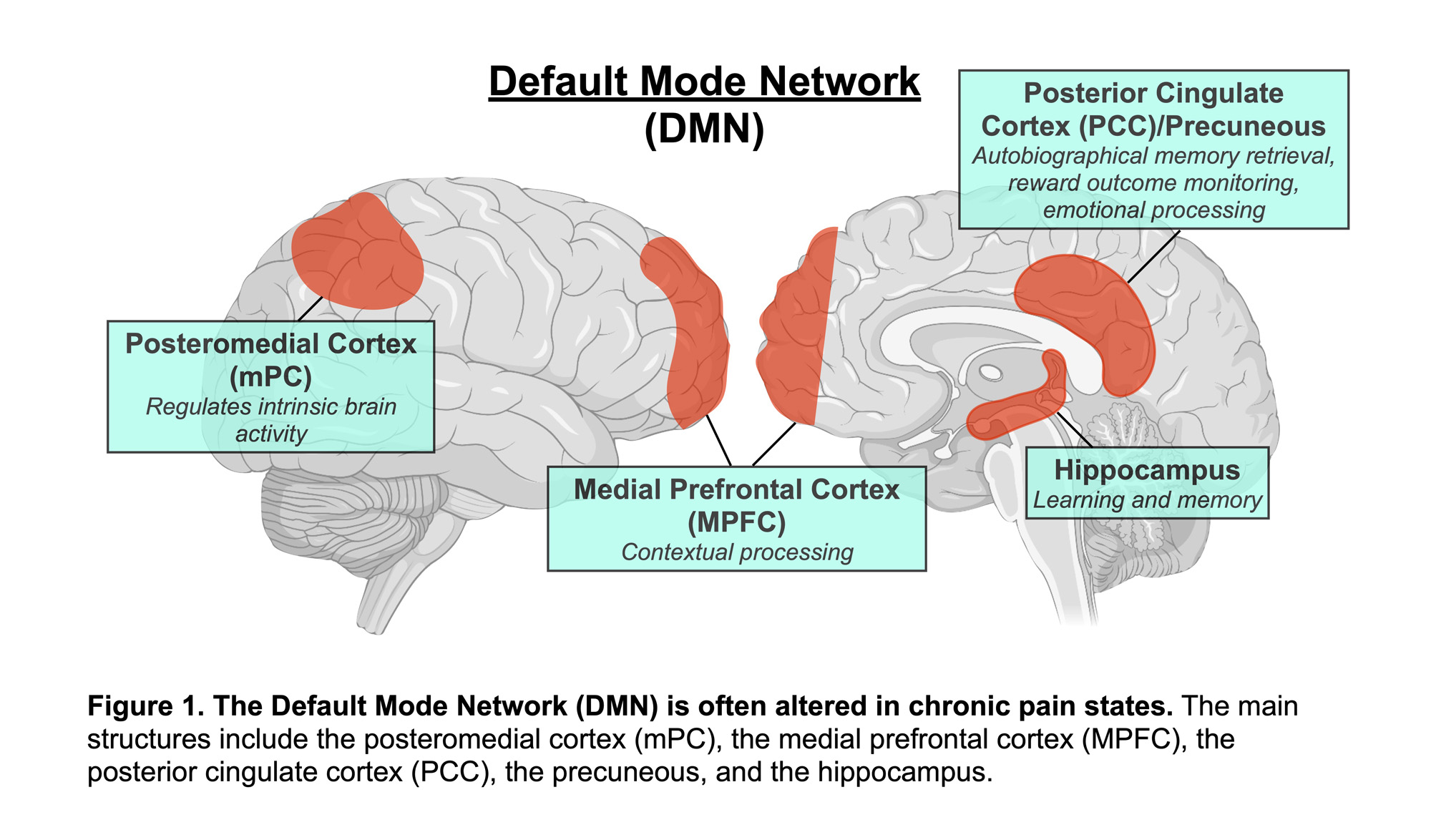
Methods: Seven patients with PsD were enrolled from the NYU Psoriatic Arthritis Center (PAC). Patients on psychotropic medications were excluded. Demographics, medical history, and medication use were recorded and focused musculoskeletal and skin exams were performed. Participants completed patient reported outcomes including the SF-36, Beck Depression Index, fatigue numeric rating score, and RAPID 3. Four healthy controls were used as a comparison group. fMRI sequences were obtained in all participants at both rest and with a fatigue inducing task (Paced Auditory Serial Addition Test) using a 3 Tesla Siemens Prisma scanner. fMRI time series were analyzed using the independent component analysis, with a focus on connectivity within the default mode network (DMN, Figure 1) which has been previously implicated in depression and chronic pain states such as fibromyalgia.
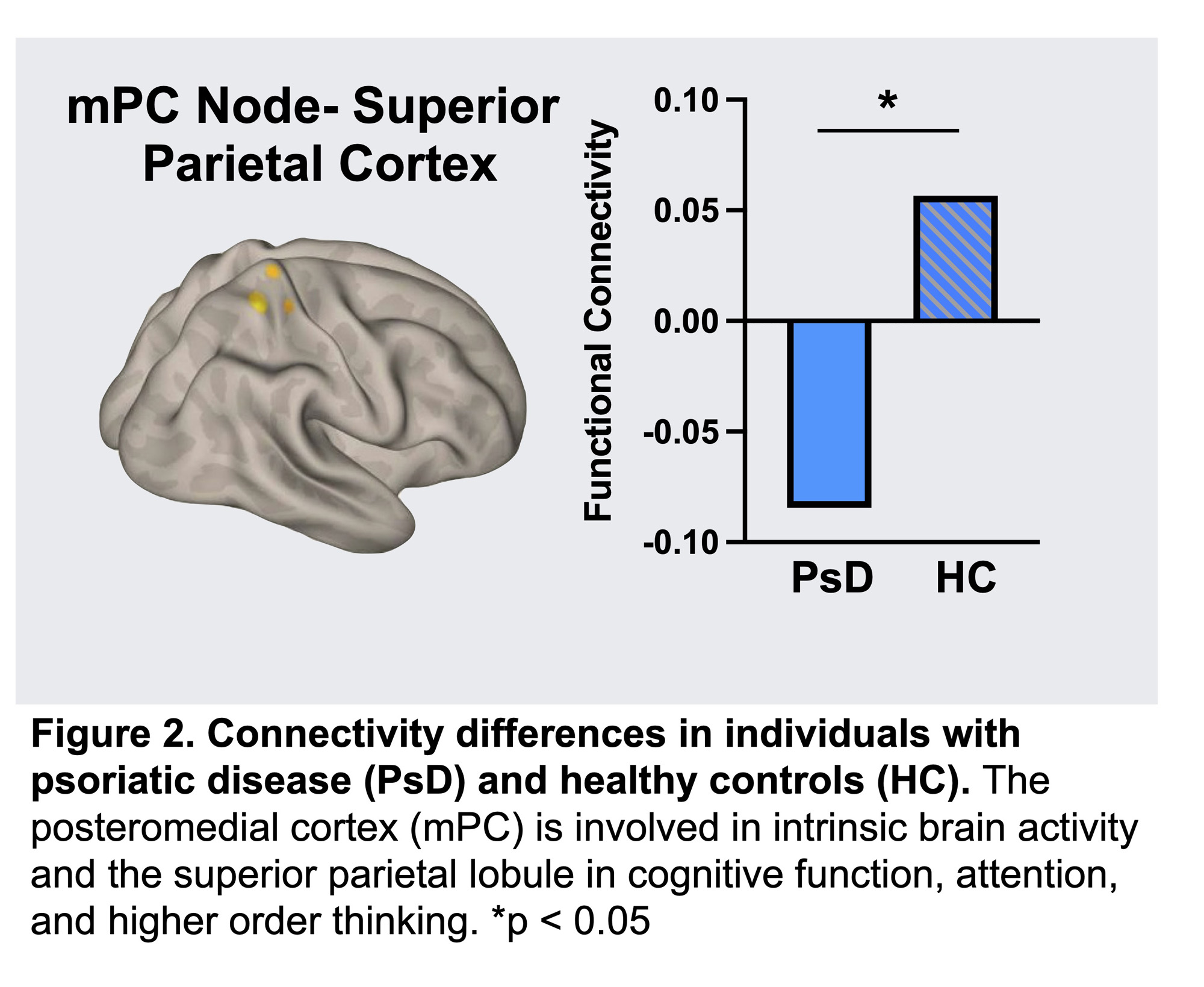
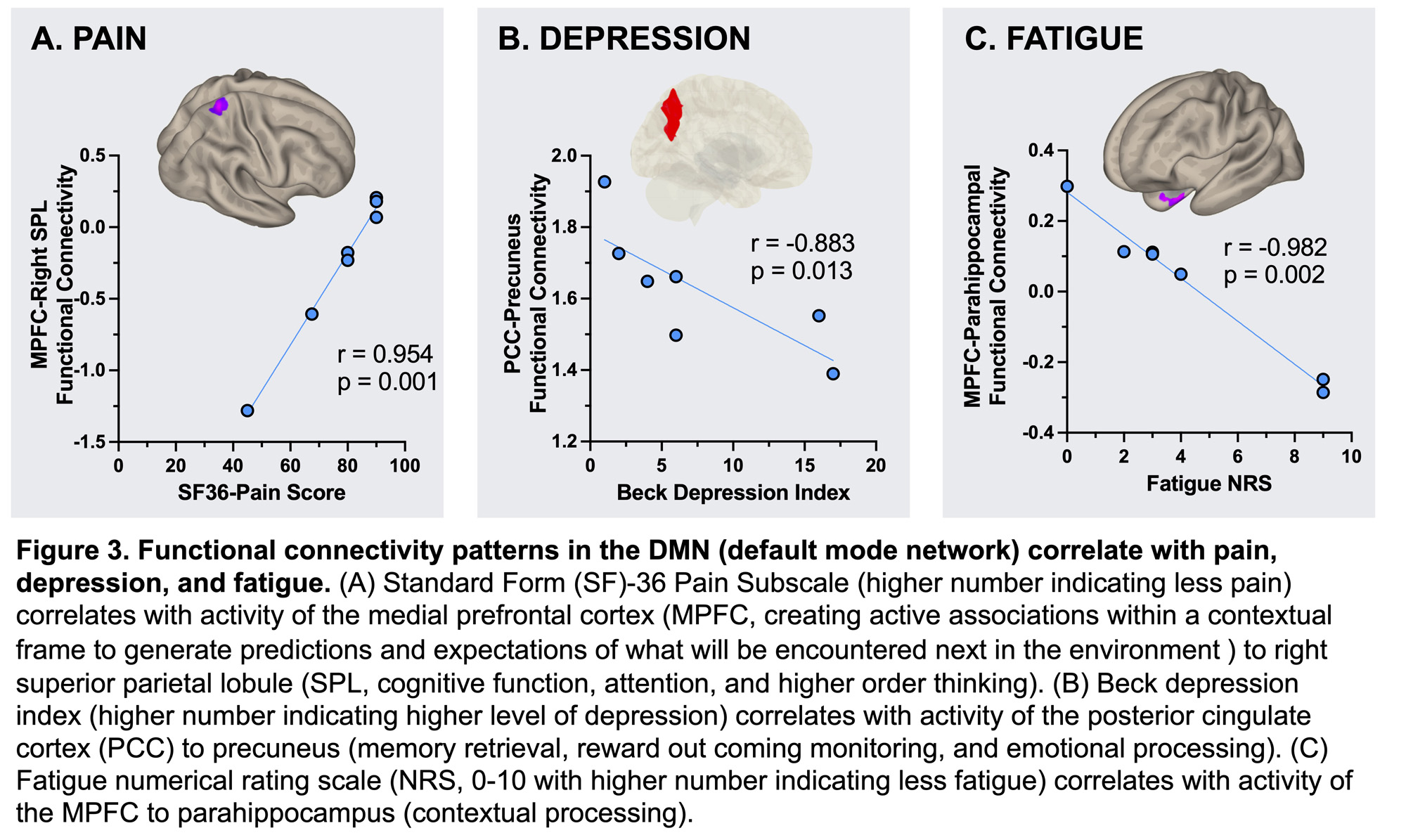
Results: Compared to healthy controls, those with PsD had decreased connectivity between the DMN’s posteromedial cortex node and the superior parietal lobule (p= < 0.05 FDR-corrected at cluster level) (Figure 2). Additionally, for the 7 participants with PsD, levels of pain, depression, and fatigue all correlated with strength of connectivity in pathways of the DMN (Figure 3).
Conclusion: This initial data demonstrates the feasibility and acceptability of using fMRI to characterize neuroconnectivity in patients with PsD. We observed differences in functional connectivity between healthy participants and patients with PsD, even with well controlled disease. Furthermore, identifying networks and connections associated with pain, depression, and fatigue may ultimately help in identifying and characterizing residual pain that contributes to worse clinical outcomes. Future studies will confirm and further characterize these findings using larger sample sizes.
To cite this abstract in AMA style:
Haberman R, Catron S, Sui Y, Moussavi S, Reddy S, Lydon E, Neimann A, Ogdie A, Lazar M, Scher J. Psoriatic Disease Associated with Neuroconnectivity Alterations in the Default Mode Network [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/psoriatic-disease-associated-with-neuroconnectivity-alterations-in-the-default-mode-network/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/psoriatic-disease-associated-with-neuroconnectivity-alterations-in-the-default-mode-network/