Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Heterotopic ossification (HO), the pathologic deposition of ectopic bone in soft tissues, is a feared complication of total hip arthroplasty (THA). HO is strongly associated with ankylosing spondylitis. However, whether rates of HO are also increased in psoriatic arthritis (PsA), another seronegative spondyloarthopathy with a predisposition to build bone, is unknown.
Methods:
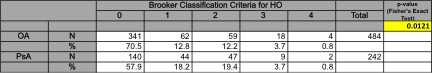
We performed a case–control study of validated PsA THA cases, each matched 2:1 on age and date of surgery with osteoarthritis (OA) controls. All THA were performed between May 2007 and June 2012. Radiographs taken ³ 6 months after surgery were reviewed to detect evidence of HO, based on Brooker classification criteria. Chart review was conducted to identify potential known risk factors for HO, which were evaluated in univariate models. A logistic regression model was constructed to evaluate independent predictors of HO. Risk factors considered for inclusion in the model were those with p-values < 0.20 from the univariate models, which were then removed in a step-wise fashion until only terms with p < 0.1 remained.
Results:
242 PsA THA were identified and matched to 484 OA controls. No PsA THA received prophylactic radiation to prevent HO. 94.2% of PsA surgeries were primary THA and 5.8% were revisions while 93.8% of OA surgeries were primary THA and 6.2% were revisions. Average age was 62.3 for PsA ± 11.7 years and 62.8 for OA ± 11.5. 55.2% of PsA were male while 44.4% of OA were male. More PsA THA than OA THA developed HO (42.2% vs. 29.6%; p-value = 0.012). In univariate models, PsA diagnosis, primary vs. revision surgery, inpatient NSAID use, ASA use, blood transfusions, sex, age, BMI, and length of stay were associated with HO. In the final logistic regression model, HO was significantly associated with PsA (OR: 1.62; 95% CI 1.16-2.27; p-value = 0.005), age (OR for each 10-year increase in age 1.15; 95% CI 1.00-1.3; p-value = 0.047), and being discharged on Coumadin for DVT prophylaxis (OR: 1.86; 95% CI 1.23-2.65; p-value = 0.0007). Inpatient Lovenox was associated with an over 4-fold increase in the odds of having HO (OR: 4.16; 95% CI 1.05-16.6; p-value = 0.043). Female gender was protective against HO (OR: 0.44: 95% CI 0.32- 0.62; p-value < 0.001).
Conclusion:
To our knowledge, this is the first study to show that psoriatic arthritis is associated with increased odds of HO following THA. Being older, receiving inpatient Lovenox, or being discharged on Coumadin also increased the risk of HO. Being female decreased the risk of developing HO. This is important information to convey to THA surgeons and patients with PsA contemplating THA.
Table 1. Incidence of heterotopic ossification
OA = Osteoarthritis; PsA = Psoriatic Arthritis
Disclosure:
M. Cedillo,
None;
A. Fein,
None;
S. M. Goodman,
None;
R. Zhu,
None;
M. P. Figgie,
None;
M. Alexiades,
None;
J. C. Burket,
None;
L. A. Mandl,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/psoriatic-arthritis-is-associated-with-heterotopic-ossification-after-total-hip-arthroplasty/