Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Glucocorticoids are recommended as short-term bridging therapy in patients with rheumatoid arthritis (RA), but as many as 30-40% of patients remain on glucocorticoids chronically. We aimed to measure the variability in the prescribing of glucocorticoids among rheumatologists and determine whether seeing a provider with a greater preference for glucocorticoids was independently associated with glucocorticoid use among patients on stable DMARD treatment.
Methods: Two cohorts were created using Medicare claims data 2006-2015. First, to measure provider variability, we identified patients with 2 diagnoses of RA within a given year who received methotrexate or a biologic. Patients could contribute to each year in which they fulfilled criteria. Among rheumatologists seeing at least 10 patients with RA in a given year, we defined the “provider preference” for glucocorticoids as the proportion of the provider’s patients receiving ≥30 days of oral glucocorticoids within 90 days of the first DMARD treatment of that year. Each year was evaluated separately to allow for changing practices over time. We then identified a separate cohort of patients with 2 diagnoses of RA who initiated methotrexate or a biologic and remained on stable DMARD therapy without biologic additions or changes for ≥6 months. We used logistic regression to determine if provider preference for glucocorticoids (measured in the larger cohort using all other patients seen by the same provider in the same year) was independently associated with a patient receiving glucocorticoids 3-6 months after the start of the DMARD course, adjusting for patient demographics, comorbidities, and healthcare utilization.
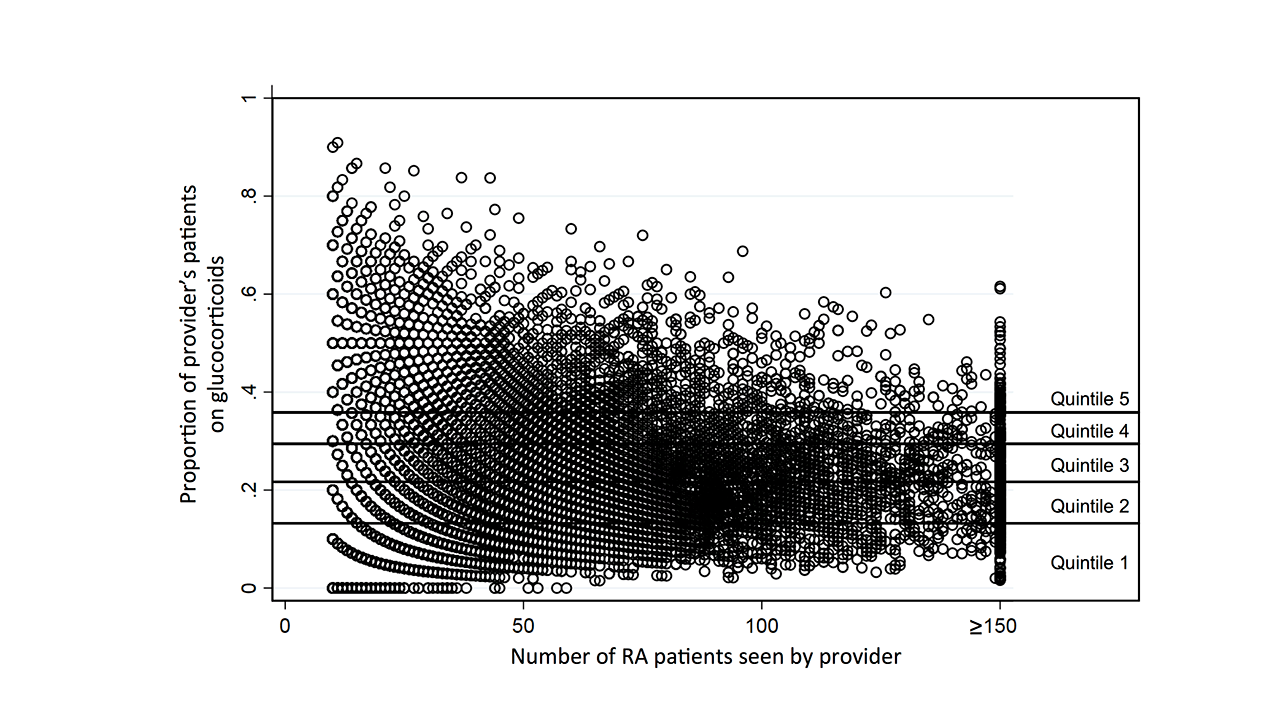
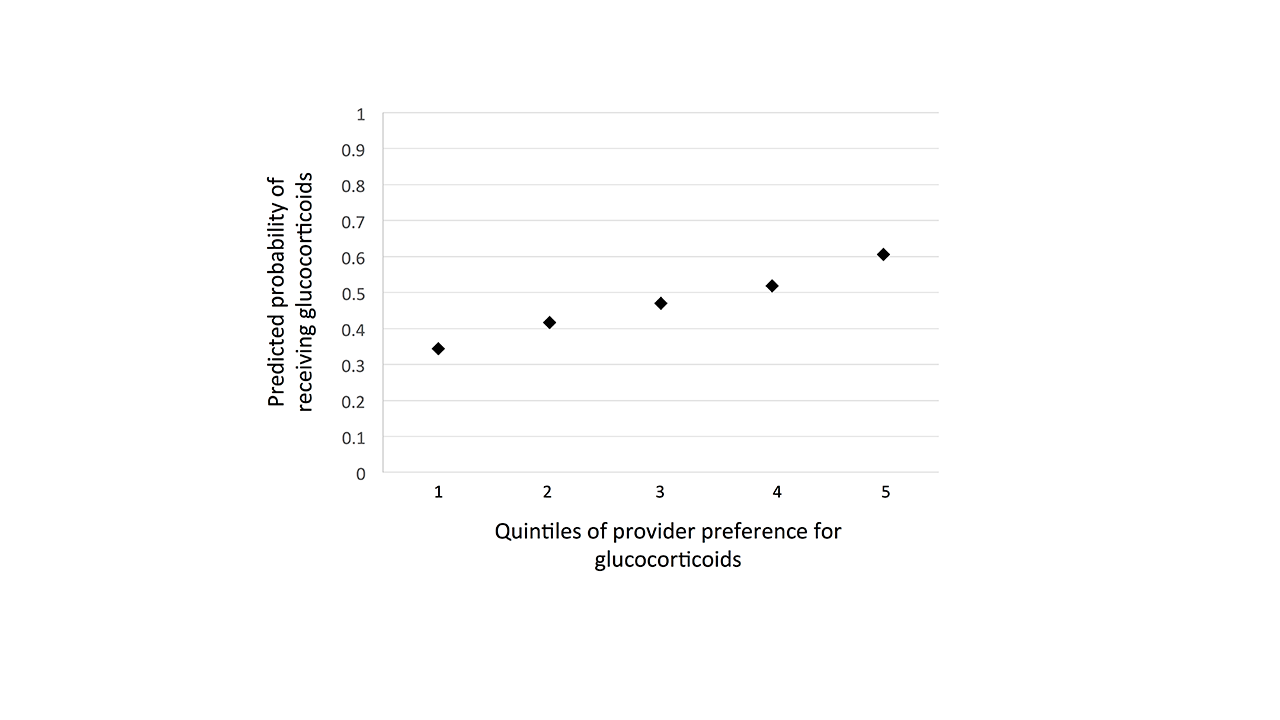
Results: We identified 1,272,644 patient-year episodes among 385,597 unique patients. Among providers seeing ≥10 patients in a given year (28,936 provider-year combinations among 6,875 providers), the proportion of a physician’s patients receiving ≥30 days of glucocorticoids was highly variable even among providers with a large patient volume (Figure 1) [median 24.3%, IQR 16.7% to 33.3%]. We identified a separate cohort of 192,614 RA patients on stable DMARD treatment for at least 6 months (47% receiving biologics) for whom we could identify the treating rheumatologist and assign a provider preference for glucocorticoids (calculated among all other patients seen by the same rheumatologist that year in the larger cohort). Provider preference for glucocorticoids was highly associated with receiving glucocorticoids 3-6 months after beginning the current DMARD course, with predicted probability ranging from 34.4% (95% CI 33.9-34.8) for patients seen by providers in the lowest quintile to 60.6% (95% CI 60.1-61.1) for those seen by providers in the highest quintile (Figure 2, all p < 0.001; first stage regression R2 0.055, F 1597).
Conclusion: Glucocorticoids prescribing practices for RA vary widely between rheumatologists. Provider preference for the use of glucocorticoids can help predict whether a patient remains on glucocorticoids during treatment. These data support the use of provider preference as an instrumental variable for epidemiologic studies evaluating glucocorticoid risk.
To cite this abstract in AMA style:
George M, Baker J, Chen L, Wu Q, Xie F, Yun H, Curtis J. Provider Variability in Glucocorticoid Prescribing for Patients with Rheumatoid Arthritis and Impact on Chronic Glucocorticoid Use [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/provider-variability-in-glucocorticoid-prescribing-for-patients-with-rheumatoid-arthritis-and-impact-on-chronic-glucocorticoid-use/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/provider-variability-in-glucocorticoid-prescribing-for-patients-with-rheumatoid-arthritis-and-impact-on-chronic-glucocorticoid-use/