Session Information
Date: Sunday, November 17, 2024
Title: Systemic Sclerosis & Related Disorders – Basic Science Poster I
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Progressive pulmonary fibrosis (ILD) is a leading cause of mortality in systemic sclerosis (SSc), particularly in the 30% of ILD patients who exhibit a progressive phenotype. Currently, there are no reliable biomarkers to timely predict worsening fibrosis and enable prompt and proportionate treatment. Extracellular vesicles (EVs) are mediators of intercellular communication that facilitate the exchange of functionally active molecules. The aim of this study was to compare the baseline proteomic, transcriptomic, and functional profiles of circulating EVs in SSc patients with progressive ILD, non-progressive ILD, and those without ILD.
Methods: Serum EVs were isolated from consecutive eligible SSc patients classified based on high-resolution computed tomography (HRCT) and INBUILD study criteria for ILD progression over a 24-month follow-up. The proteome and transcriptome of the EVs were characterized using proximity extension assays (Olink) and RNA sequencing. Serum EV’s were used to stimulate the lung epithelial cell line A549, lung fibroblasts and primary monocytes isolated from healthy patient blood. Protein and RNA were isolated from these cells and epithelial-mesenchymal transition (EMT) markers were screened by western blot and qPCR.
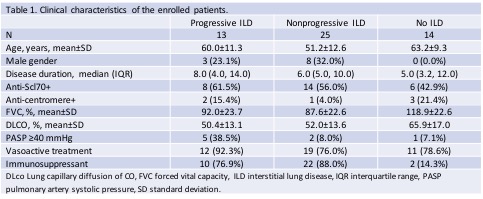
Results: Clinical characteristics of the 52 enrolled SSc patients are presented in Table 1. Proteomic and transcriptomic comparisons revealed differences in the abundance of proteins and RNAs involved in EMT processes, extracellular matrix metabolism, angiogenesis, vesicle trafficking, and immune response. Moderate EMT (measured via analysis of vimentin (2.21 fold), N cadherin (1.32 fold), twist (2.09 fold), and snail (1.74 fold) protein and transcript levels) was induced in A549 epithelial cells after direct exposure to EVs from progressive SSc-ILD patients but not from SSc patients without ILD. Interestingly the SSc sera exosomes activated primary monocytes (as characterised through increased TNF-α (2.19 fold) and STAT1 (1.96 fold) levels) and these activated monocytes induced EMT in downstream lung epithelial cells.
Conclusion: Circulating EV characteristics vary according to the presence and prognosis of ILD in SSc patients and these EVs were capable of driving EMT in lung epithelial cells directly and indirectly via immune cells.
To cite this abstract in AMA style:
De Lorenzis E, Koeppen K, Di Donato S, Dibb S, Klein E, Wasson C, Del Galdo F. Proteomic, Transcriptomic, and Functional Characterization of Circulating Extracellular Vesicles in Progressive Scleroderma Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/proteomic-transcriptomic-and-functional-characterization-of-circulating-extracellular-vesicles-in-progressive-scleroderma-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/proteomic-transcriptomic-and-functional-characterization-of-circulating-extracellular-vesicles-in-progressive-scleroderma-interstitial-lung-disease/