Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriasis is a chronic inflammatory disease of the skin and is often accompanied by arthritis. The underlying pathogenesis of psoriasis is still unclear, but T-helper 1 (Th1) and Th17 cells are thought to play important roles. Mucosal-associated invariant T (MAIT) cells are innate lymphocytes that are restricted by MHC-related molecule-1 (MR1), express a semi-invariant TCRa chain: Va7.2-Ja33 in humans and Va19-Ja33 in mice. Previously, we have shown that MAIT cells inhibited the progression of autoimmune encephalomyelitis (EAE), and the inhibition of EAE was accompanied by reduced autoreactive Th1 and Th17 responses. Therefore, we sought to investigate whether MAIT cells have a suppressive role in an animal model of psoriasis by using MR1-/- mice lacking MAIT cells.
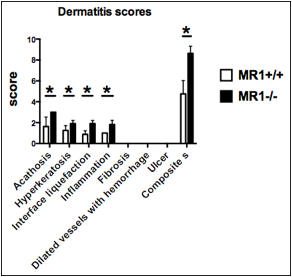
Methods: A murine imiquimod (IMQ)-induced model of psoriasis (J Immunol. 2009; 182: 5836-45) was induced in MR1-/- and MR1+/+C57BL/6J mice at 8 to 10 weeks of age. Mice were topically treated with 62.5mg of 5% IMQ cream (Mochida Pharmaceutical) on the shaved back for 5 consecutive days. Mice were injected with 500ml of phosphate-buffered saline on day 1 and 3. The severity of skin inflammation was monitored every day, and scored by usning linical Psoriasis Area and Severity Index (PASI) score. Erythema, scaling, and thickening of the back skin were scored on the scale from 0 to 4. (J Immunol. 2009; 182: 5836-45). Skin samples were stained with haematoxylin-eosin, and the severity were graded on a scale of 1 to 3 for acanthosis; 1 to 2 for hyperkeratosis, interface liquefaction, inflammation, dermal cellularity, presence of dilated vessels with hemorrhage; 0 to 1 for ulcer or erosion. Differences between groups were assesed using the Mann-Whitney U test, and the significance level was set at p < 0.05.
Results: Both MR1-/- and MR1+/+C57BL/6J mice equally developed erythema. MR1-/-C57BL/6J mice displayed significantly severe scales and thickness of the back skin than MR1+/+ mice. The histopathological analysis revealed there was a significant worsening of dermatitis and the higher dermatitis score in MR1-/- mice compared to control MR1+/+C57BL/6J mice.
Conclusion: The present study indicated that MAIT cells play a suppressive role for the development of psoriasis. In humans, MAIT cells have recently been found in normal and psoriatic skin. Although further verification for mechanisms of the function of MAIT cells for pathogenesis of psoriasis, regulation of MAIT cell functions may become a novel therapeutic strategy for psoriasis. 
To cite this abstract in AMA style:
Murayama G, Chiba A, Toda H, Yamaji K, Tamura N, Miyake S. Protective Role of Mucosal-Associated Invariant T (MAIT) Cells in an Imiquimod-Induced Psoriasis Model [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/protective-role-of-mucosal-associated-invariant-t-mait-cells-in-an-imiquimod-induced-psoriasis-model/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/protective-role-of-mucosal-associated-invariant-t-mait-cells-in-an-imiquimod-induced-psoriasis-model/