Session Information
Date: Saturday, November 16, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Myositis-associated interstitial lung disease (MA-ILD) is a complex condition with a variable prognosis and diverse clinical manifestations. The 2022 ATS/ERS/JRS/ALAT criteria for PPF provide a standardized framework for assessing disease progression, highlighting the emerging role of progressive pulmonary fibrosis (PPF) in patient outcomes. We aim to identify prognostic factors associated with mortality in patients with MA-ILD and to evaluate the impact of PPF on survival.
Methods: We conducted a longitudinal cohort study of patients with MA-ILD. From December 2018 to February 2022, we prospectively enrolled 41 patients and followed up with them until February 2024. The diagnosis of inflammatory myositis was made according to the Bohan and Peter criteria for dermatomyositis and polymyositis and the Sontheimer criteria for clinically amyopathic dermatomyositis. Baseline demographic, clinical, and pulmonary function data were collected. PPF was diagnosed and classified using the 2022 ATS/ERS/JRS/ALAT guideline criteria. The presence of PPF at the 1-year follow-up and the Gender-Age-Physiology (GAP) index score were assessed as potential predictors of mortality. The impact of PPF on mortality in MA-ILD was analyzed using Mann-Whitney U tests, Chi-square tests, and Fisher’s exact tests. Survival analysis was performed using Kaplan-Meier methods and log-rank tests.
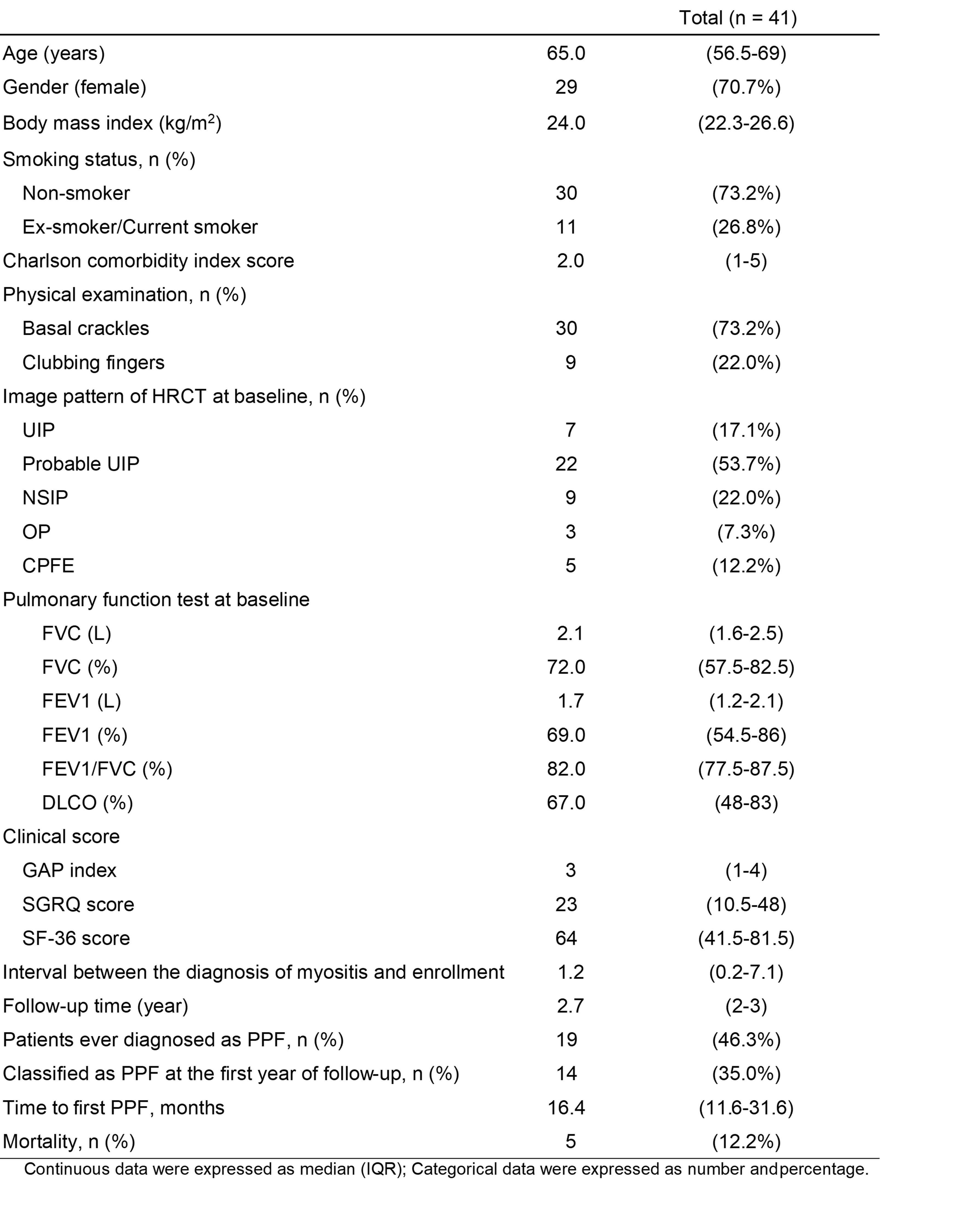
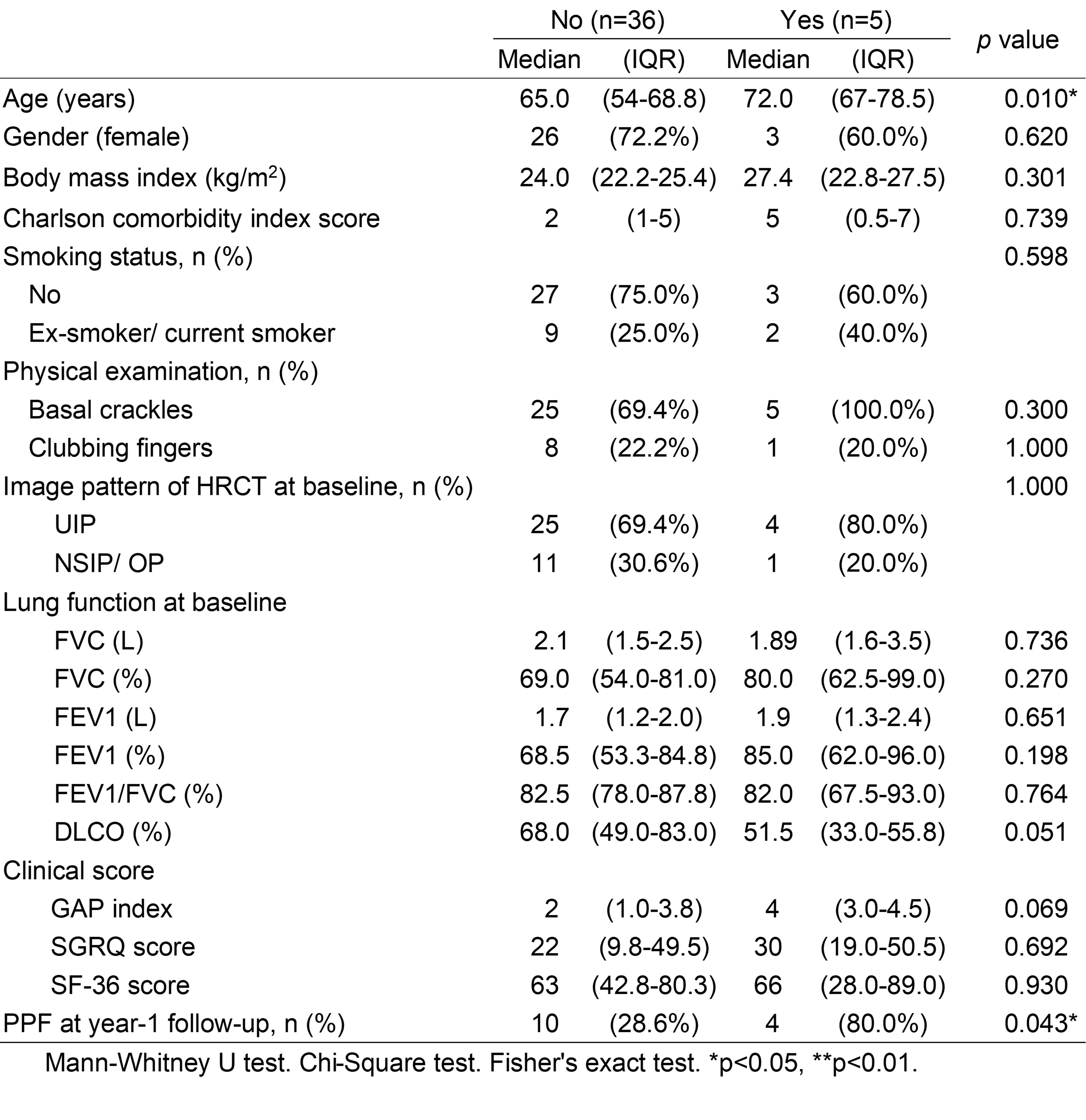
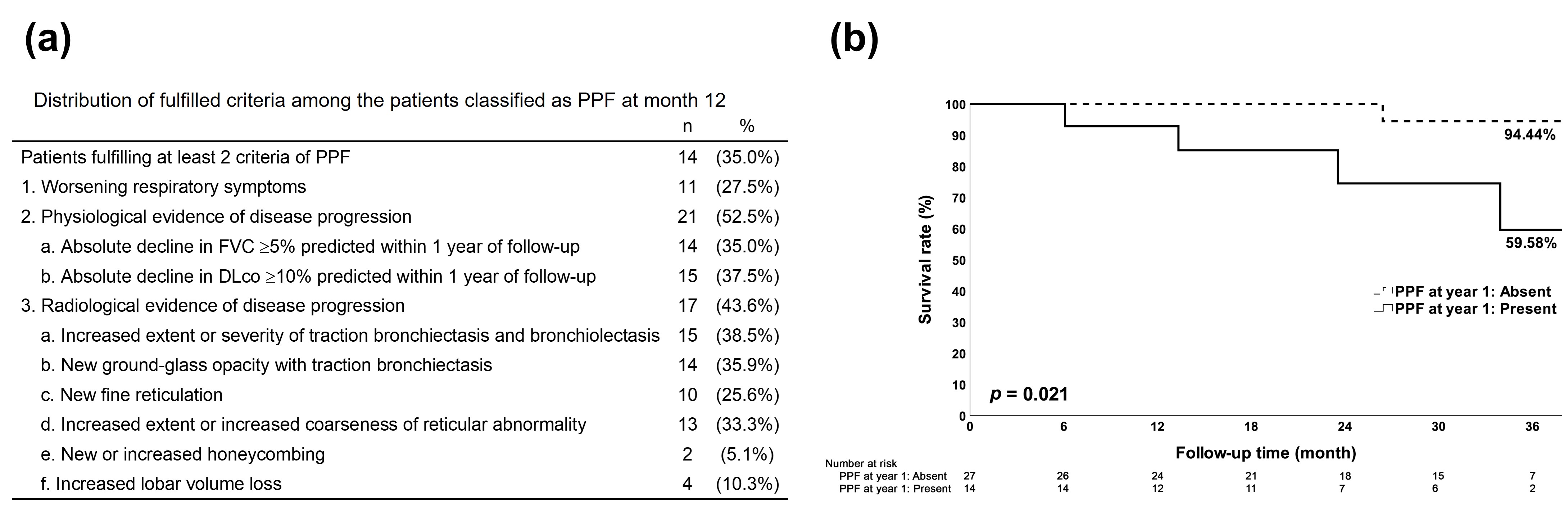
Results: Demographic and clinical data collected at baseline are shown in Table 1. The median age of the cohort was 65 years (IQR 56.5-69), and 70.7% were female. The most common HRCT patterns at baseline were probable UIP (53.7%) and NSIP (22.0%). Table 2 shows the comparison between survival and mortality subgroups. Patients who died during the follow-up period (n=5) were significantly older compared to survivors (median age 72 vs. 65 years, p=0.010). Figure 1a demonstrates the distribution of fulfilled PPF criteria among patients classified as PPF at month 12, with radiological evidence of disease progression being the most common criterion (52.5%). The presence of PPF at year 1 was significantly associated with mortality (80.0% in the mortality group vs. 28.6% in the survival group, p=0.043). Kaplan-Meier analysis (Figure 1b) demonstrated a significant difference in survival between patients with and without PPF at year 1 (log-rank p=0.021), with a 3-year survival rate of 59.6% and 94.4%, respectively.
Conclusion: The presence of PPF at the 1-year follow-up is a significant predictor of mortality in patients with MA-ILD. Radiological evidence of disease progression is the most common criterion fulfilled among patients classified as PPF. These factors may be useful for risk stratification and guiding management decisions in this patient population. Early identification of PPF and close monitoring of high-risk patients may help improve outcomes in MA-ILD.
To cite this abstract in AMA style:
Liao Y, Liu M, Fu P, Huang W. Progressive Pulmonary Fibrosis Predicts Mortality in Myositis-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/progressive-pulmonary-fibrosis-predicts-mortality-in-myositis-associated-interstitial-lung-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/progressive-pulmonary-fibrosis-predicts-mortality-in-myositis-associated-interstitial-lung-disease/