Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: The occurrence of interstitial lung disease (ILD) in the course of systemic sclerosis (SSc) is associated with increased morbidity and mortality. SSc-ILD evolution is heterogeneous. Most studies have focused on the evolution of forced vital capacity (FVC), without considering other components of ILD progression. Recent efforts to define progressive fibrosing (PF)-ILD have led to a common definition (2022 ATS Clinical Practice Guidelines), including patient’s symptoms, pulmonary function tests, and radiologic criteria for progression, occurring over a one-year period. For SSc, it has recently been proposed to apply these criteria without a time limit (2024 ATS Clinical Practice Guidelines). Using a cohort of well-characterized SSc-ILDs with consecutive lung HRCT, we aimed to decipher disease evolutionary trajectories.
Methods: The study population consisted of adult patients with a SSc according to ACR-EULAR 2013 classification criteria, and an ILD diagnosed on HRCT at the Avicenne Hospital (Bobigny, France) between January 2006 and December 2022. Patients without any interpretable follow-up HRCT were excluded. All baseline and follow-up HRCTs were centrally reviewed by an expert radiologist. An unsupervised hierarchical clustering was performed on progression modalities. PF-ILD criteria (ATS 2022) were applied considering a limited period of 1-year or no time limit.
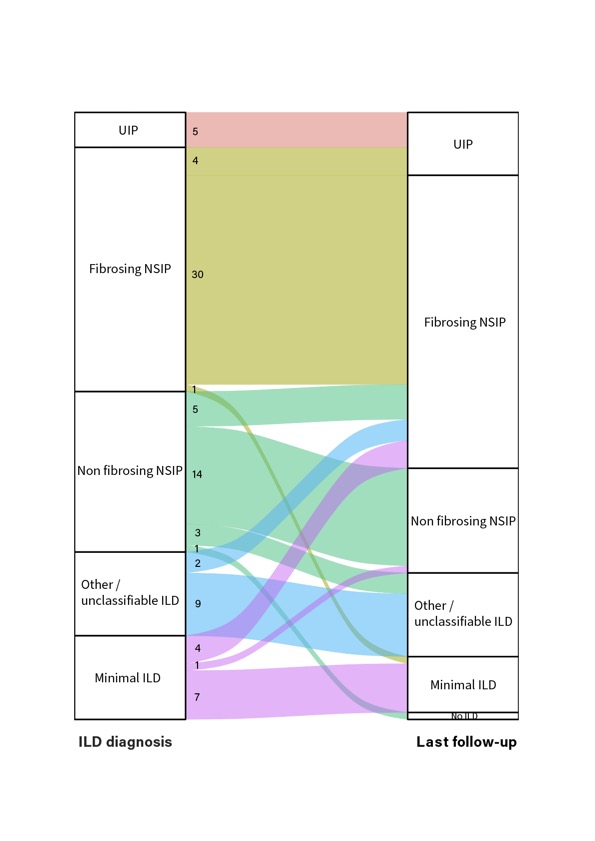
Results: Our cohort consisted of 87 SSc-ILD patients (78.2% female, 19.5% diffuse cutaneous disease, 46% anti-topoisomerase I antibodies positive). At ILD diagnosis, the patterns were: usual interstitial pneumoniae (UIP) (5.7%), non-specific interstitial pneumoniae with radiologic evidence of fibrosis (fNSIP) (40.2%), NSIP without evidence of fibrosis (nfNSIP) (26.4%), other ILD pattern (13.8%) and minimal ILD lesions (13.8%). During follow-up, 25.3% of patients experienced a pattern change. The most common changes were from nfNSIP to fNSIP (n=5), from minimal ILD to fNSIP (n=4), and from fNSIP to UIP (n=4). Radiographic progression criteria were met in 57.5%. We clustered patients into 3 groups of radiologic evolution: cluster 1 never had new ground glass opacities (GGO) but frequently presented increased extent or increased coarseness of reticular abnormalities (83%), increased extent or severity of traction bronchiectasis (67%), and increased lobar volume loss (67%); cluster 2 had new GGO with traction bronchiectasis (100%), associated or not with other radiologic progression criteria (clusters 2a and 2b); cluster 3 rarely showed signs of radiologic progression (< 5% for each modalities). In 78 patients with concomitant HRCT and PFT on at least one follow-up visit, the cumulative incidence of progression at 5 years was 25.4% using a 1-year definition and 48.1% using a definition with no time limit. Transplant-free and overall survival were significantly altered in the group of patients who met the 1-year progression criteria (fast progressors), in contrast to slow progressors, whose survival did not differ significantly from that of non-progressors.
Conclusion: Identifying these subgroups of SSc-ILD progression modalities could assist in classifying patients and guiding treatment decisions.
To cite this abstract in AMA style:
Roeser a, Brillet P, Boubaya M, Caux F, Dhote R, Nunes H, Uzunhan Y. Progression Patterns in Systemic Sclerosis – Associated Interstitial Lung Diseases [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/progression-patterns-in-systemic-sclerosis-associated-interstitial-lung-diseases/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/progression-patterns-in-systemic-sclerosis-associated-interstitial-lung-diseases/