Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Previous studies have reported higher risk of thyroid disease in patients with giant cell arteritis (GCA) and ANCA-associated vasculitis (AAV) compared to age- and sex-matched controls. The aim of this study was to compare the risk of hypothyroidism or hyperthyroidism in patients with large-vessel vasculitis (giant cell arteritis, GCA and Takayasu’s arteritis, TAK), polyarteritis nodosa (PAN), and AAV.
Methods: Patients GCA, TAK, PAN, granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA) enrolled in a prospective, multicenter, longitudinal study were included. All patients were followed with standardized data collection. Information on type of thyroid disease was systematically collected for each form of vasculitis. Odds ratios (OR) and 95% confidence intervals (CI) for risk of thyroid diseases were calculated between clinical subgroups.
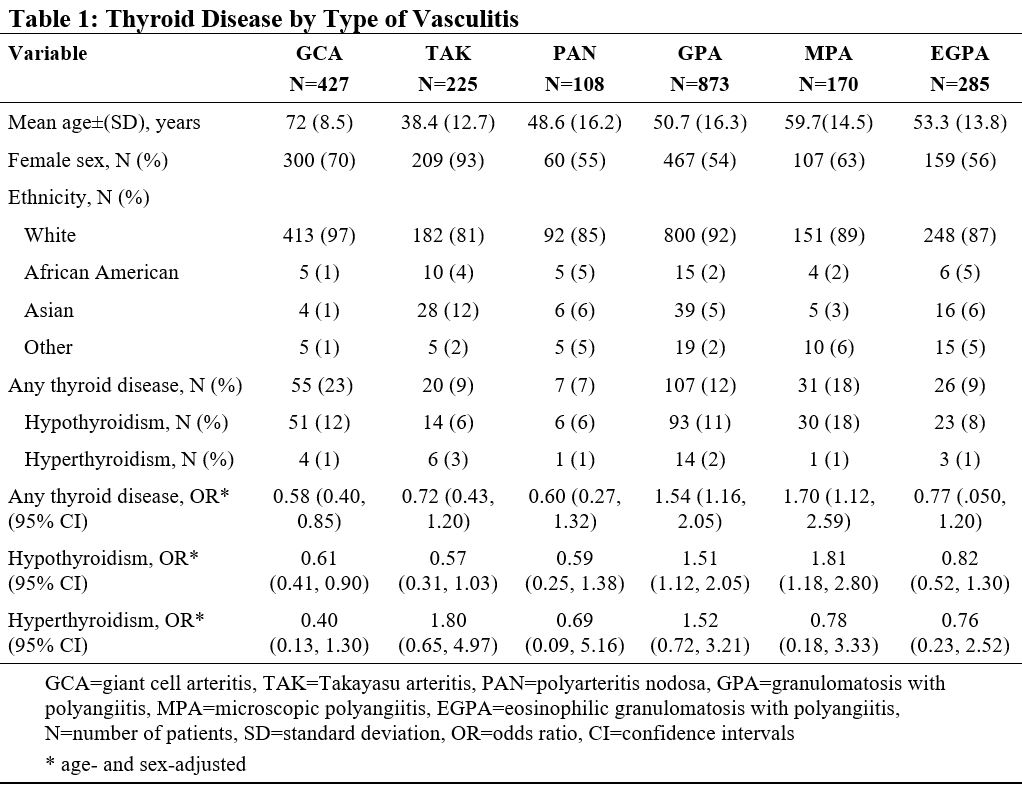
Results: The study included 2,087 patients, 63% female, 90% White, mean age 54.6 (±17.2) years. Diagnoses were: GCA (427, 20%), TAK (225, 11%), PAN (108, 5%), GPA (873, 42%), MPA (170, 8%), and EGPA (285, 14%).
Thyroid disease was present in 246 patients (12% overall cohort), 83% female, mean (±SD) age 59.2 (14.8) years. The majority of the cases were hypothyroidism; 217 patients (88% with thyroid disease). The frequency of thyroid disease by type of vasculitis, and, age- and sex-adjusted OR for thyroid disease is in Table 1. Adjusting for age and sex, patients with LVV had lower risk of hypothyroidism (OR 0.59, 95% CI 0.42, 0.81) while risk of hypothyroidism was higher in patients with AAV (OR 1.80, 95% CI 1.31, 2.47). Patients with GCA had the lowest risk compared to the other forms of vasculitis while patients with GPA and MPA had the highest risk (Table 1). There were no differences in age- and sex-adjusted risk of hyperthyroidism between the different forms of vasculitis (Table 1).
Conclusion: There are important differences in the risk of hypothyroidism, but not hyperthyroidism, between the different forms of vasculitis. Patients with GCA have the lowest age- and sex- adjusted risk of hypothyroidism while patients with GPA and MPA had the highest risk. Possible explanations for these findings include differences in genetic susceptibilities, immune responses, or treatment exposures between the forms of vasculitis. The interplay of thyroid disease and vasculitis warrants further investigation.
To cite this abstract in AMA style:
Kermani T, Cuthbertson D, Carette S, Khalidi N, Koening C, Langford C, McAlear C, Monach P, Moreland L, Pagnoux C, Seo P, Specks U, Sreih A, Warrington K, Merkel P. Prevalence of Thyroid Disease Among Patients with Vasculitis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-thyroid-disease-among-patients-with-vasculitis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-thyroid-disease-among-patients-with-vasculitis/