Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic, multi-organ, autoimmune disease whose prevalence in the US has not been recently updated in real-world studies. Prevalence estimates range from 50-150 per 100,000 adults in the US, but these estimates are due to be refreshed. In addition, the heterogeneity of the clinical manifestations of SLE and lack of a diagnostic test make SLE prevalence challenging to quantify. Therefore, our study sought to utilize recent nationally representative population data to estimate prevalence estimates of SLE in the US.
Methods: We analyzed data from the 2016 – 2018 Medical Expenditure Panel Surveys (MEPS), an annual survey using a complex sampling strategy to represent the US civilian non-institutionalized population. Prevalence was defined as self-reported SLE diagnosis with additional SLE-related medication use and/or any rheumatologist visit during the calendar year. Two other SLE diagnostic criteria were used as a sensitivity analysis (sensitive: SLE diagnosis only; restrictive: SLE diagnosed and currently treated). Self-reported SLE was linked to a specific visit to a healthcare professional (outpatient or inpatient). The annual prevalence was reported per 100,000 US adults and 95 % confidence interval (CI) stratified by key demographic characteristics.
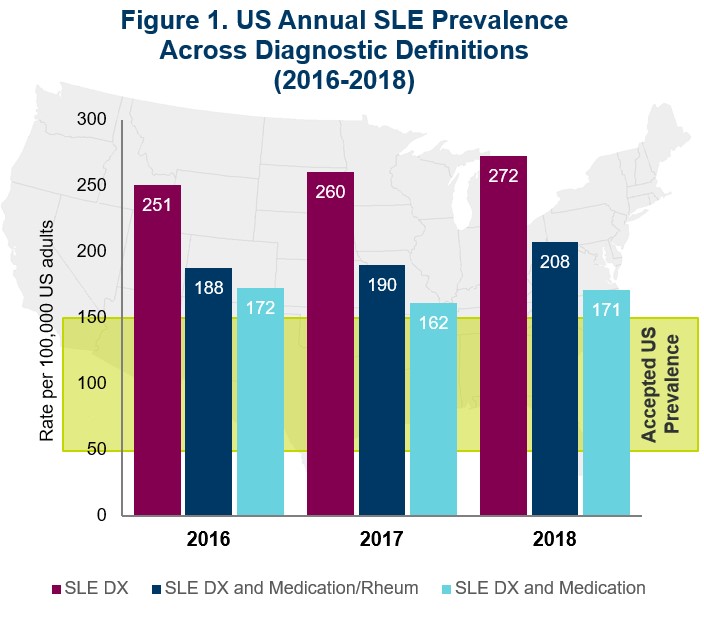
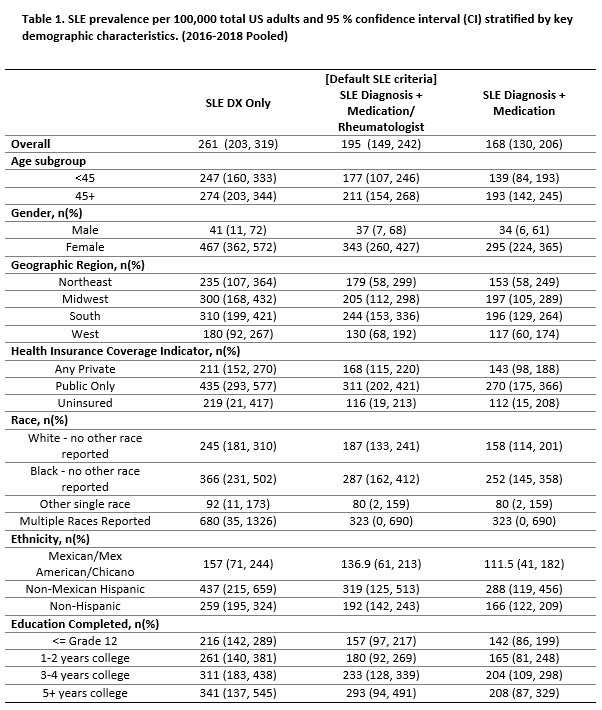
Results: From 2016-2018, 96,996 adults reported annual data in MEPS, of which 199 (0.20%) reported SLE diagnosis, 154 (0.16%) respondents report SLE with either SLE-related medication and/or rheumatologist visit, and 139 (0.14%) respondents reported SLE with SLE-related medication. The pooled weighted annual prevalence of SLE using each respective SLE-definition was 261 ( 95% CI: 203, 319); 195 (95% CI: 149, 242) and 168 (95% CI: 130, 206) per 100,000 adults. From 2016 to 2018, the prevalence of SLE appeared to increase slightly. The prevalence of SLE was about 9 times higher in females compared to males (343 vs. 37 per 100,000 adults). Individuals who reported Black or multiple races and Mexican Hispanic ethnicity appeared to have a higher prevalence of SLE compared to white or non-Hispanic adults, respectively. Respondents with public insurance (Medicare or Medicaid) were twice as likely to report SLE than those privately insured (311 vs. 168 per 100,000 adults). Respondents in the Southern region of the US had a slightly higher prevalence of SLE compared to other regions (North, West, or East). The 95% confidence intervals were relatively wide across most stratified analyses, limiting the ability to detect population differences.
Conclusion: The self-reported SLE prevalence in the US was higher across all three disease definitions in MEPS than the currently accepted estimate of 50 to 150 per 100,000 adults. Similar to other studies, females, Black, and Hispanic respondents were found to have a higher prevalence of SLE compared to males and white or non-Hispanic individuals. While many real-world studies include only single-payer populations, we demonstrate a more diverse payer patient-population and a higher burden of SLE. SLE prevalence is challenging to quantify; however, this study suggests that the actual US of SLE prevalence may be higher than reported.
To cite this abstract in AMA style:
Pollack M, Sze-jung Wu S, Farrelly E, Grabich S, Ortmann R. Prevalence of Systemic Lupus Erythematosus in the United States: Updated Population Representative Estimates from the Medical Expenditure Panel Survey (MEPS) 2016-2018 [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-systemic-lupus-erythematosus-in-the-united-states-updated-population-representative-estimates-from-the-medical-expenditure-panel-survey-meps-2016-2018/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-systemic-lupus-erythematosus-in-the-united-states-updated-population-representative-estimates-from-the-medical-expenditure-panel-survey-meps-2016-2018/