Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Self-reported poor sleep is common in SLE, but few studies have objectively measured sleep have been conducted. In general population studies, sleep disorders are associated with poor health outcomes relevant to SLE, including lower pain thresholds and higher rates of depression, cognitive impairment, systemic inflammation, and cardiovascular events. We report on the prevalence of objectively-measured sleep disturbances in an SLE cohort, examine whether patient-reported measures of sleep correspond with objective measures, and analyze the association of sleep disturbances with patient-reported outcomes.
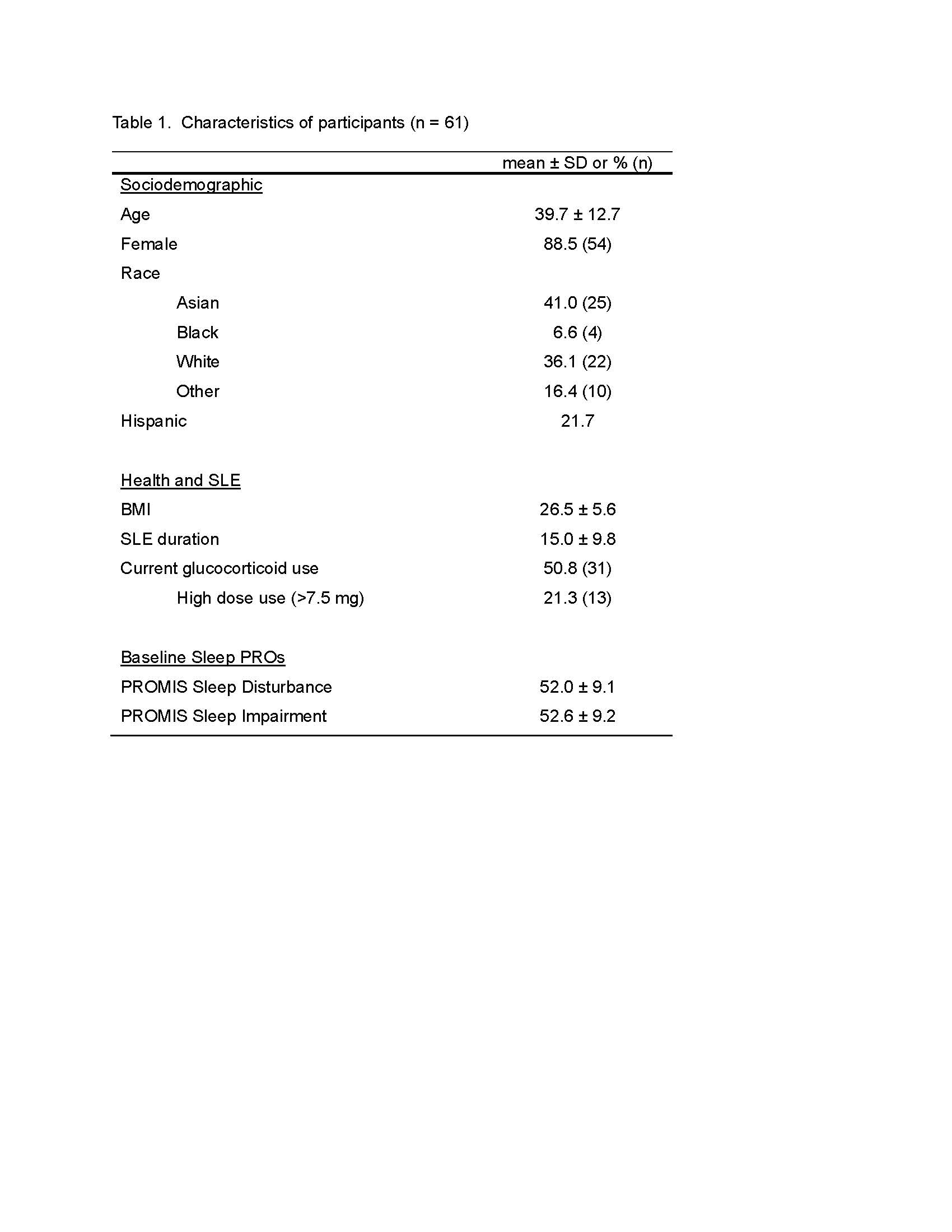
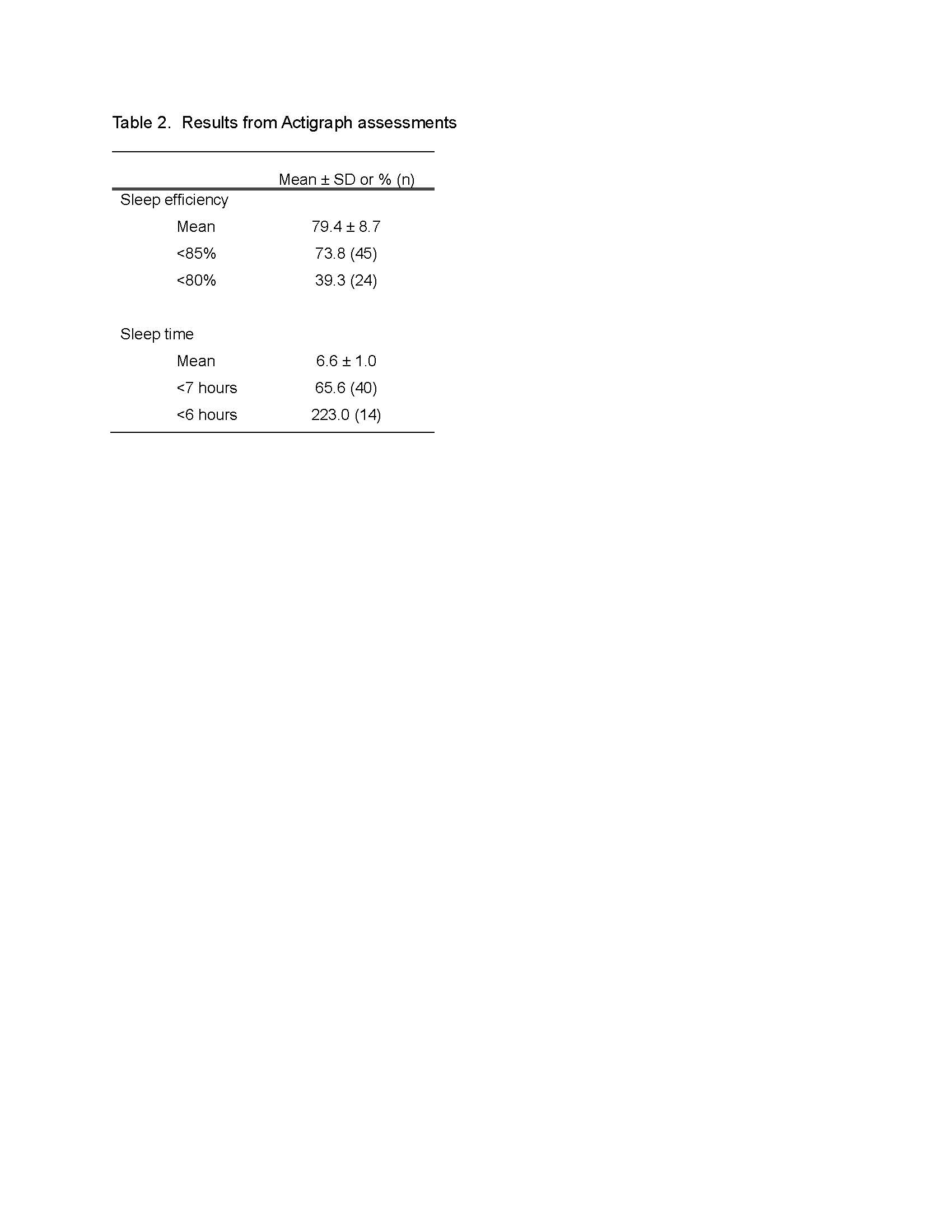
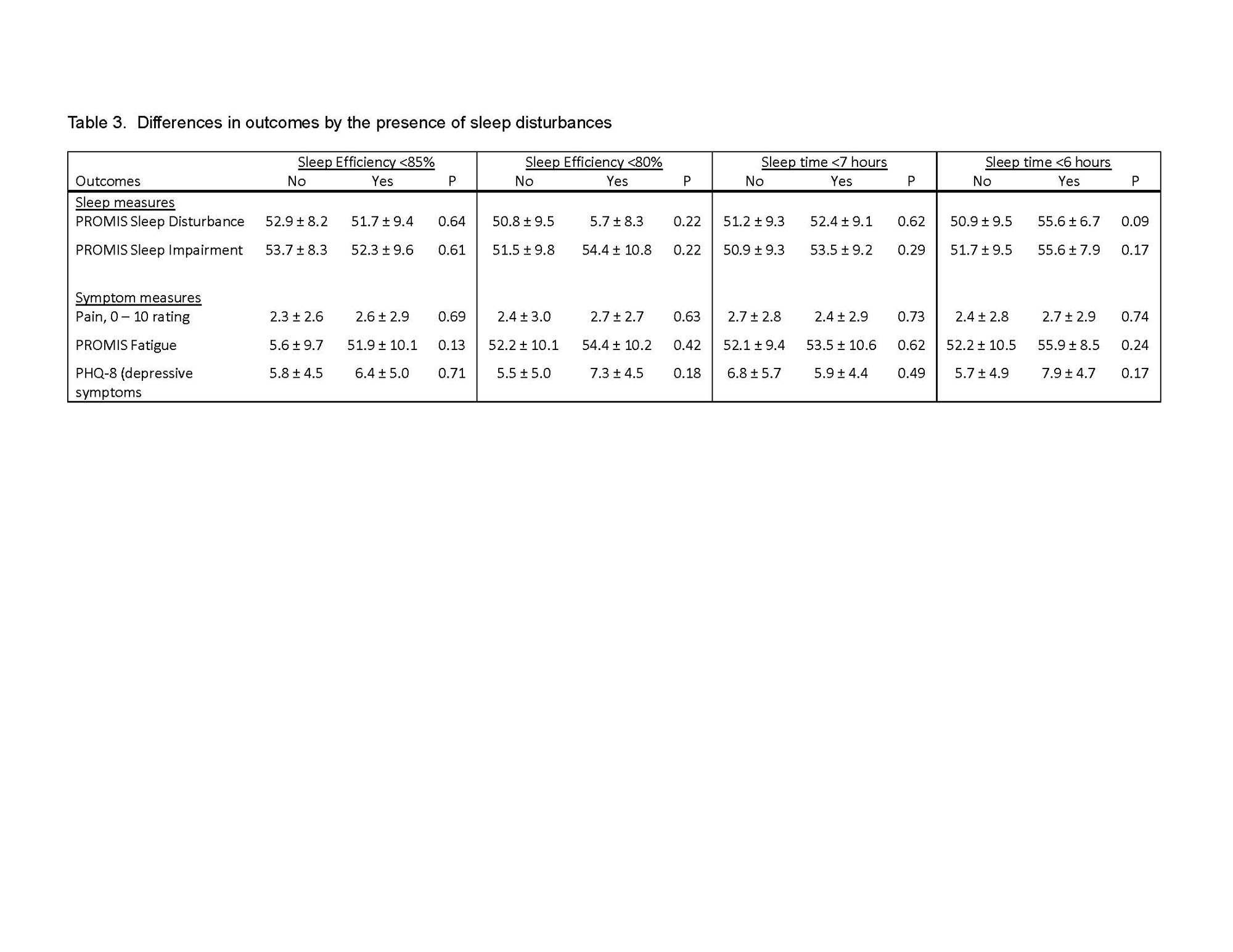
Methods: All participants were drawn from the California Lupus Epidemiology Study (CLUES). A subset of CLUES participants (n = 61) who received their SLE care at our institution participated in a sleep study and underwent 7 nights of home sleep monitoring via actigraphy (GT9X, Actigraph Corp., Pensacola, FL), as well as concurrent interviews in which patient-reported outcome measures (PROMs) of sleep (PROMIS Sleep Disturbance and Sleep Impairment) and symptoms (pain rating 0-10, PROMIS Fatigue, and depressive symptoms [Patient Health Questionnaire, PHQ-8]) were collected. Actigraphs yielded estimates of time in bed, time asleep, and sleep efficiency (time asleep/time in bed).We examined 2 indicators of sleep disturbance: poor sleep efficiency and short sleep. Poor sleep efficiency was defined as < 85% (the standard criterion) and < 80%.Short sleep time was defined as < 7 hours (based on CDC guidance) and < 6 hours. Analyses examined differences in PROMs by each sleep disturbance indicator.
Results: Participant characteristics are shown in Table 1.Mean sleep efficiency was 79.4% ± 8.7%, 74% had sleep efficiency < 85%, and 39% had sleep efficiency < 80% (Table 2). Mean sleep time was 6.6 ± 1.0 hours, 66% had sleep time < 7 hours, and 23% had sleep time < 6 hours. Sleep PROM scores were generally within 0.5 SD of the population mean, not reflecting the high prevalence of objective sleep disturbance in the sample. There were no significant differences in the sleep or symptom PROMs by any of the sleep disturbance indicators (Table 3).
Conclusion: Overall, objective sleep disturbances measured by actigraphy were common in this cohort. However, these results were discordant with self-reported sleep PROMs, which were similar to the general population. The lack of differences in sleep or symptom PROMs by sleep disturbance may be due to our relatively small sample. It is also possible that if sleep disturbances are of long duration, individuals’ perceptions of the effects sleep disturbances may have normalized. If findings are replicated, research will be needed to identify more sensitive methods of measuring sleep disturbances in SLE by patient report.
To cite this abstract in AMA style:
Katz P, Yazdany J, Dall'Era M. Prevalence of Objectively Measured Sleep Disturbance in Systemic Lupus Erythematosus (SLE) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-objectively-measured-sleep-disturbance-in-systemic-lupus-erythematosus-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-objectively-measured-sleep-disturbance-in-systemic-lupus-erythematosus-sle/