Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with SLE experience a high burden of various comorbidities at disease onset and during disease progression. Studies of excess morbidity prior to SLE diagnosis are limited. We thus estimated the cumulative prevalence of common comorbidities (defined by validated morbidity indices) in incident SLE patients before SLE diagnosis and compared it with matched population comparators in Denmark.
Methods: Patients ≥18years of age with a first registration of SLE (defined by International Classification of Diseases (ICD) codes) from Jan 1, 1996 to July 31, 2018 in the Danish National Patient Register (DNPR), and who had no SLE ICD codes prior to 1996 were identified. For a registration of SLE to qualify for the case definition, it had to be a primary or secondary SLE ICD code from rheumatology, nephrology or dermatology departments (inpatient or outpatient) or a primary SLE ICD code from any inpatient department. The first-ever SLE registration was set as SLE diagnosis date (the index date), and the case definition fulfillment date was used for matching. Patients with >12 months between these dates were excluded. Up to 19 comparators per SLE case, matched by age and sex, were selected from the general population. ICD-coded diagnoses during outpatient and inpatient care were retrieved from the DNPR and DNPR-Psychiatry. To identify comorbid conditions, the initial date of diagnosis from DNPR based on ICD codes or the date of the first prescription filled for osteoporosis, hypertension, or diabetes, were used. We estimated cumulative prevalence and prevalence ratios (PR) with corresponding 95% confidence intervals (CI) of morbidities as defined by Charlson, Elixhauser, and SLICC-ACR damage indices at 10, 5, 2, and 1 year before and at index date in SLE patients and the population comparators, adjusted for age and sex.
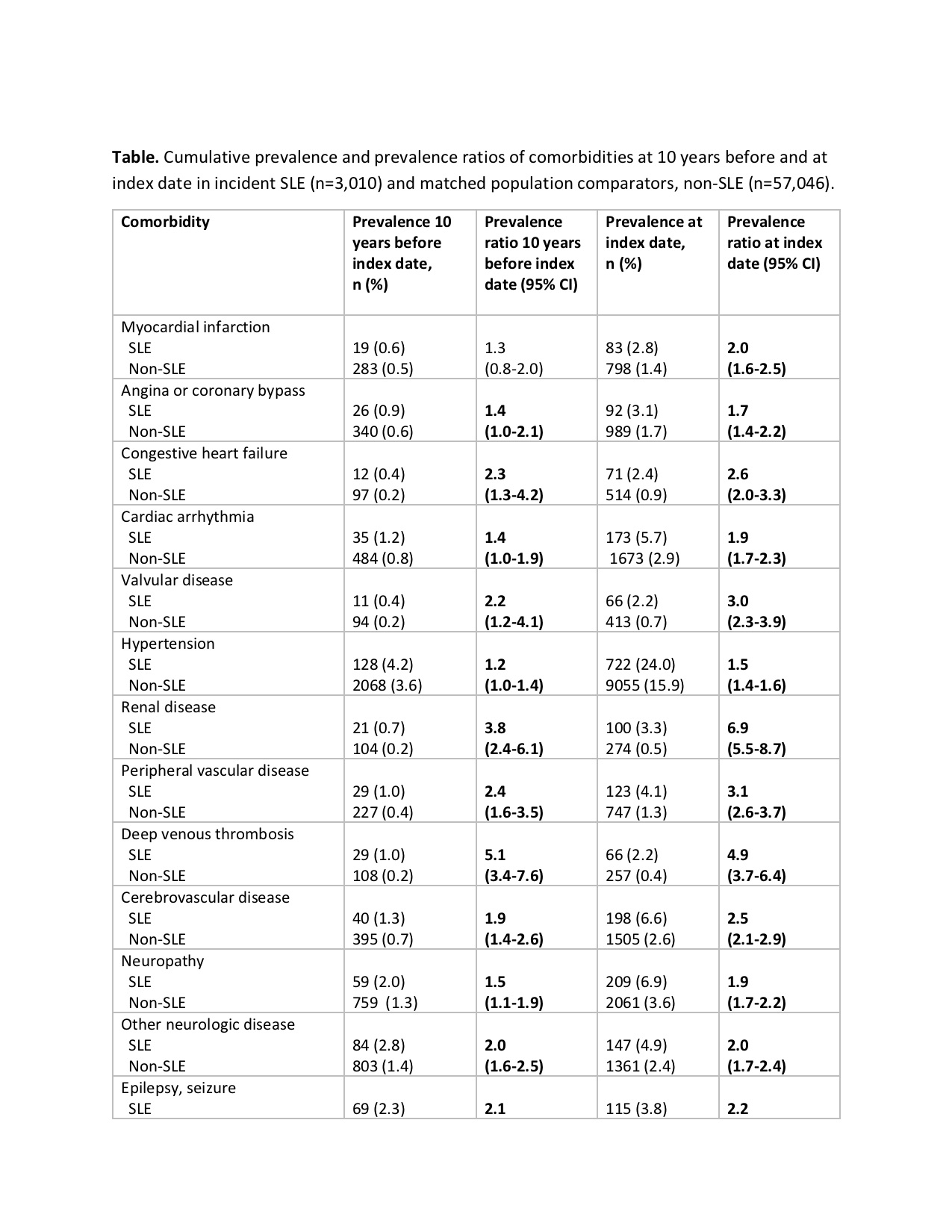
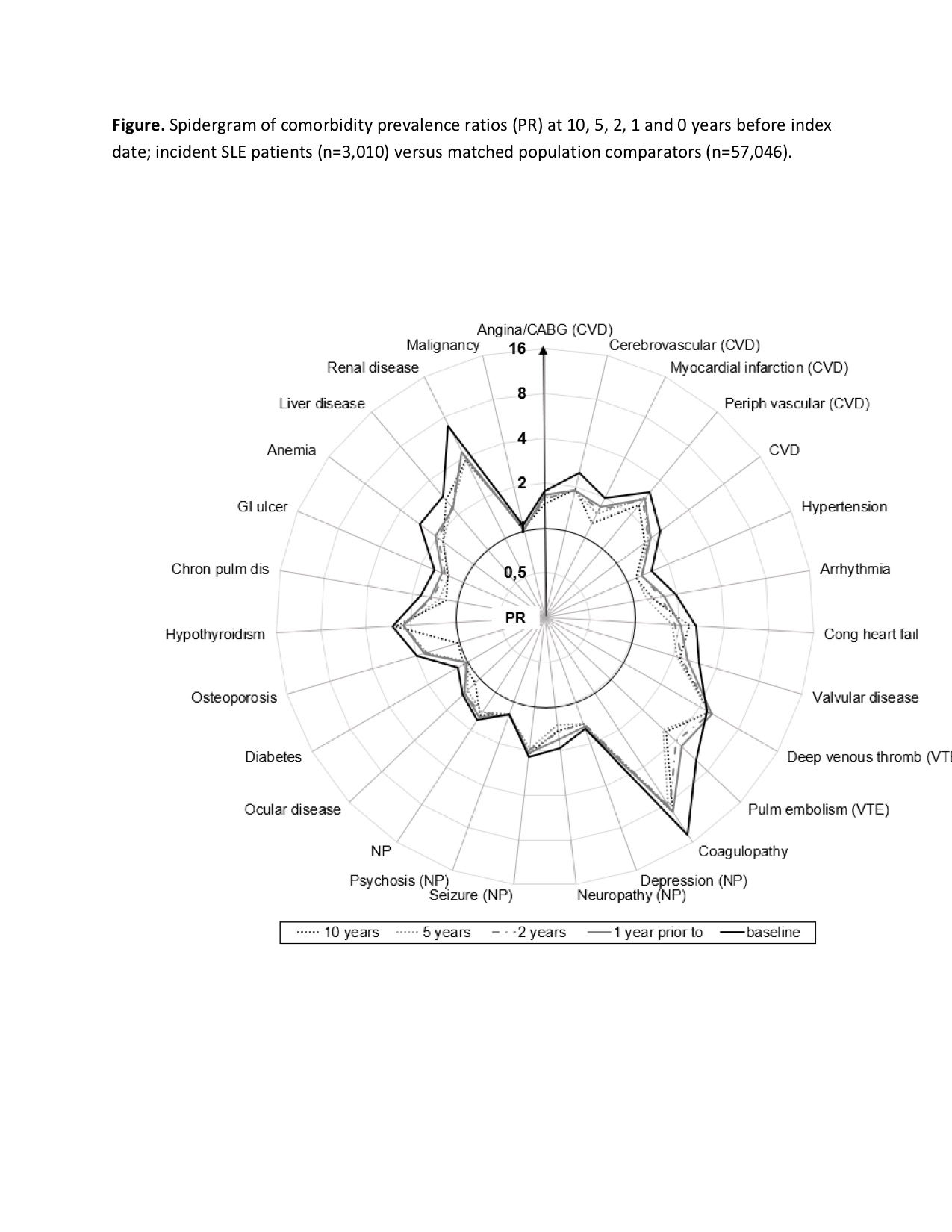
Results: 3,010 patients with incident SLE were matched to 57,046 population comparators. 84% of the subjects were female; the mean age at index date was 47 years. Except for malignancy, all morbidities appeared more prevalent 10 years before index date or at index date compared to the population comparators (Table). The PRs were particularly high for venous thromboembolic events, coagulopathy, valvular diseases, and renal diseases with PRs ranging from 3.0 to 14. Also, cardiovascular, neurologic, hematologic, gastrointestinal, and endocrine diseases were significantly overrepresented before the index date. A striking finding is the stability of the overrepresentation for the mentioned morbidities even 10 years before index date among SLE patients as depicted in the Figure.
Conclusion: We found a higher than expected prevalence of multiple morbidities – not only at the time of SLE diagnosis but also during the 10-year pre-diagnosis period among the individuals with incident SLE. These findings may have implications on our understanding of SLE pathogenesis and the subsequent accumulation of morbidity after SLE diagnosis. In a clinical setting, these findings underscore the importance of a broad screening for various comorbidities at SLE diagnosis as early awareness and treatment of multimorbidity is expected to improve outcomes in SLE.
To cite this abstract in AMA style:
Simard J, Faurschou M, Jacobsen S, Hansen R. Prevalence of Morbidity Prior to Diagnosis of Incident Systemic Lupus Erythematosus in the Danish Population [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-morbidity-prior-to-diagnosis-of-incident-systemic-lupus-erythematosus-in-the-danish-population/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-morbidity-prior-to-diagnosis-of-incident-systemic-lupus-erythematosus-in-the-danish-population/