Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes Poster I: Multimorbidity
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The aim of our study was to assess the prevalence of migraine and neuropathic pain in a sample of patients with chronic inflammatory rheumatism (CIR) routinely followed in Rheumatology and to compare it with that found in the general French population.
Methods: Patients with rheumatoid arthritis (RA), ankylosing spondylitis (AS) and psoriatic arthritis (PsA) were invited to complete a validated self-assessment questionnaire. Migraine was diagnosed according to the IHS migraine diagnostic criteria. Neuropathic pain was retained in case of a total score at 3 or more at DN4-interview questionnaire. Continuous parameters were compared between independent groups (RA/AS/PsA, with/without migraine, with/without neuropathic pain) with the ANOVA or Student t-test. Categorical data were compared between groups with the chi-squared test or Fisher’s exact test. Binary variables of particular interest, like the presence/absence of migraine or pain, were evaluated with generalized linear models (i.e., logistic regression). Differences between our cohort and the French general population were expressed as ORs, based on the Mantel-Haenszel method.
Results: A total of 499 patients with CIR were included (238 RA, 188 AS and 72 PsA and one patient not classified). We found a prevalence of migraine of 34% (165/484). This prevalence was higher in PsA patients (32/71: 45.1%). Parameters associated with a higher prevalence of migraine were a higher level of anxiety (OR=1.14 [1.05-1.23]), female sex (OR=4.03 [2.24-7.52]), younger age (OR=0.97 [0.95-0.99]), TNF alpha inhibitors treatment (OR=1.91 [1.14-3.23]) in the entire population and a high disease activity in AS patients. Systemic inflammation was never significantly associated. Among the 165 patients with migraine, 124 (75.2%) had HIT-6 scores above 55, which indicated that headache had an important impact on these patients.
Chronic pain with neuropathic characteristics was found in 21.5% of 493 patients with CIR. The intensity of pain was moderate (5.0 ± 1.5). Prevalence was significantly higher in the AS group (26.7%) than in the PsA (19.4%) and RA (17.6%) groups (p = 0.02). Active disease (OR = 1.00, 95%CI: 1.00-1.03), and salazopyrine treatment (OR = 1.91. 95%CI: 1.08-12.9) were associated with a higher risk of neuropathic pain.
Compared to the general population, our cohort showed significantly higher rates of migraine (OR = 1.91, 95%CI: 1.57-2.32) and neuropathic pain (OR = 3.71, 95%CI: 2.97-4.62), based on the Mantel-Haenszel method. We observed significant differences in strict and probable migraine rates between the general population and our cohort, when we performed separate analyses, according to gender and age. The higher frequency of neuropathic pain in our sample compared to the general population was more dramatic among younger patients but was not different between the sexes.
Conclusion: We found a high prevalence of migraine and neuropathic pain in our sample of patients with rheumatic disease. It seems therefore important to check the presence of migraine or neuropathic pain in rheumatic disease patients with residual pain despite a clinically well-controlled rheumatic disease.
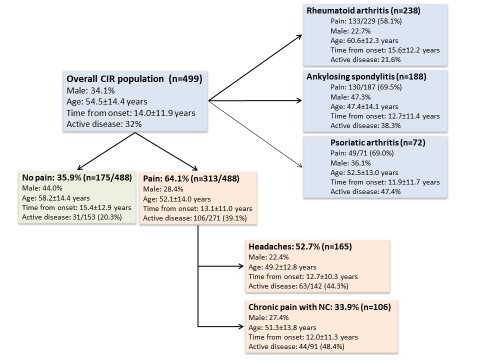 Distribution of rheumatic diseases, migraine, and neuropathic pain among study participants.
Distribution of rheumatic diseases, migraine, and neuropathic pain among study participants.
To cite this abstract in AMA style:
Mathieu S, Couderc M, Pereira B, Dubost J, Malochet-Guinamand S, Tournadre A, Soubrier M, Moisset X. Prevalence of Migraine and Neuropathic Pain in Rheumatic Disease [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-migraine-and-neuropathic-pain-in-rheumatic-disease/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-migraine-and-neuropathic-pain-in-rheumatic-disease/
