Session Information
Date: Monday, November 13, 2023
Title: (1082–1099) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Quality of care (QoC) in SLE patients has been studied by Schmajuk et al. (Arthritis Care Res2022), who developed six quality measures assessing blood pressure, lupus nephritis screening, hydroxychloroquine prescription, and corticosteroid dosing. In this study, prompted by the increased loss to follow up and disruption in care associated with the COVID-19 pandemic, we quantify the effect of loss to follow up from the rheumatology clinic at University Hospital Brooklyn (UHB) on QoC of our SLE patients.
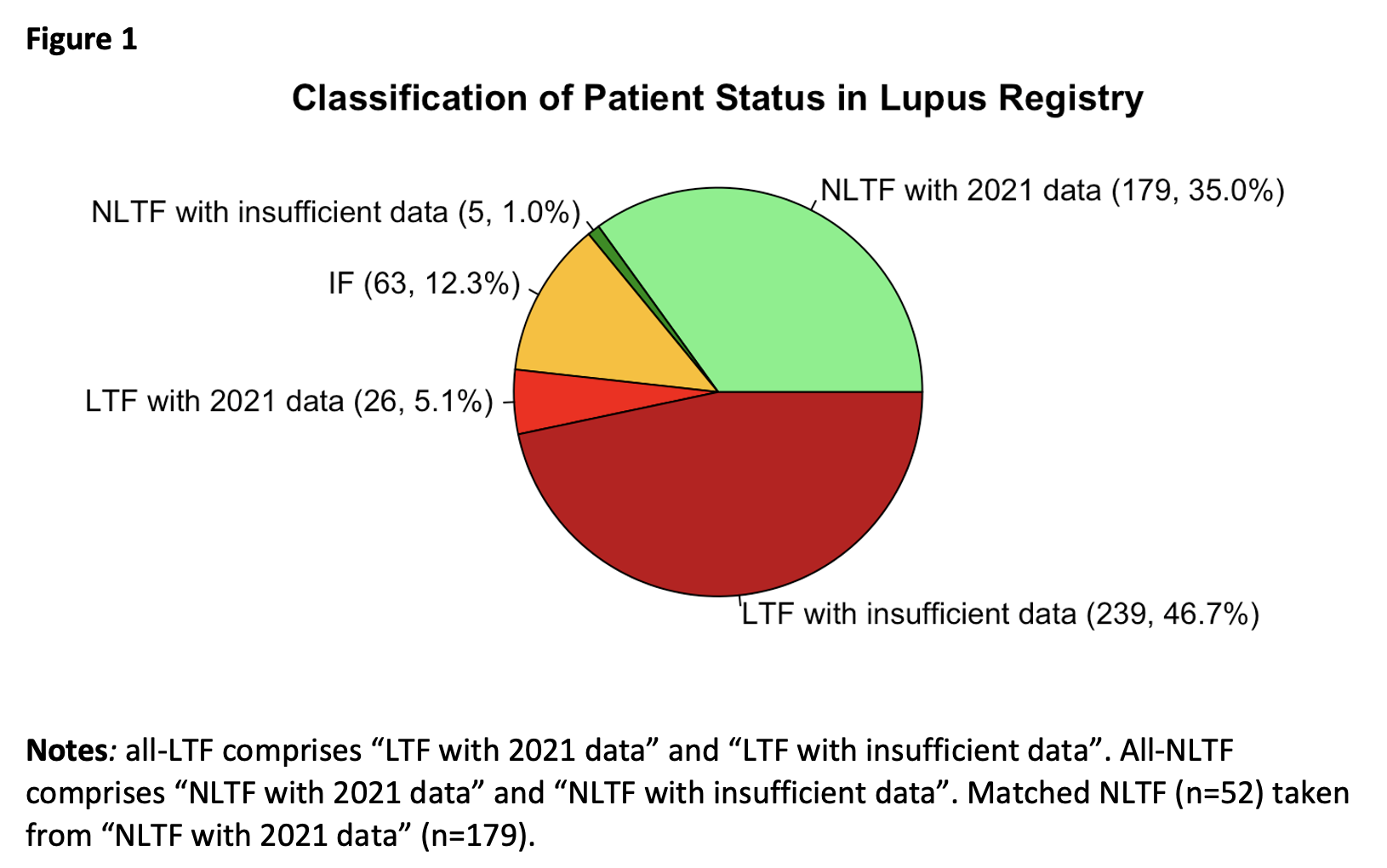
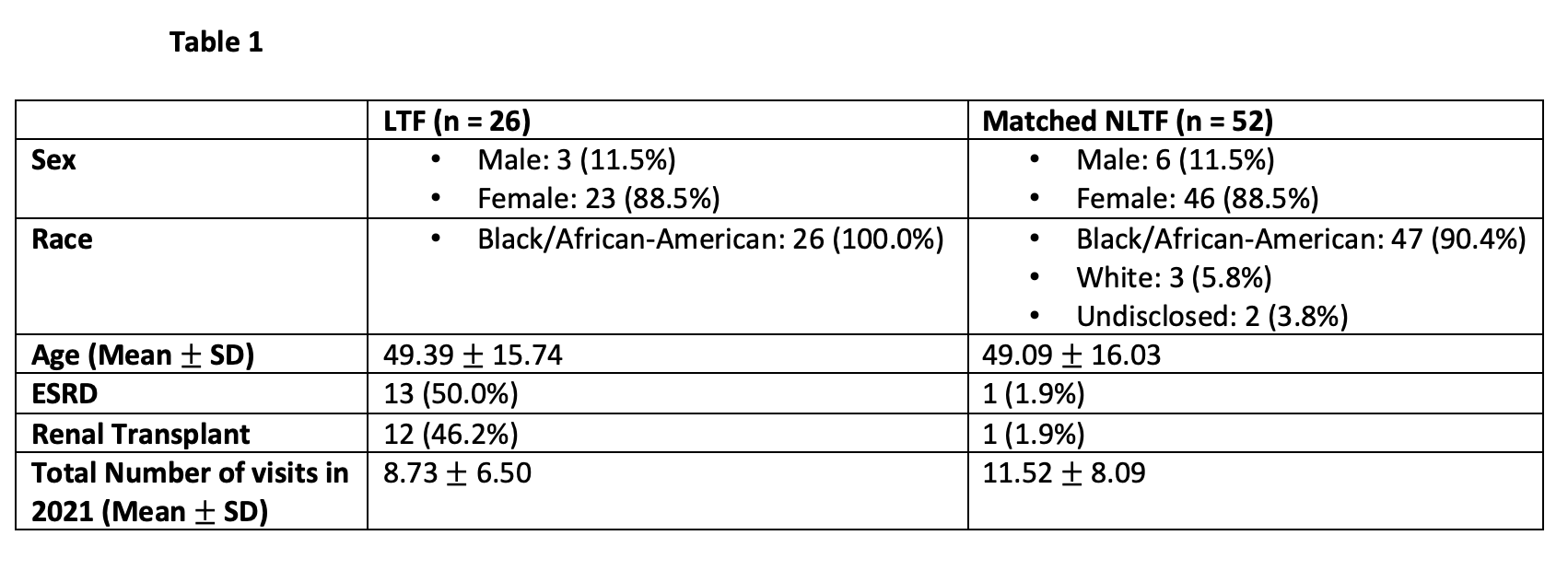
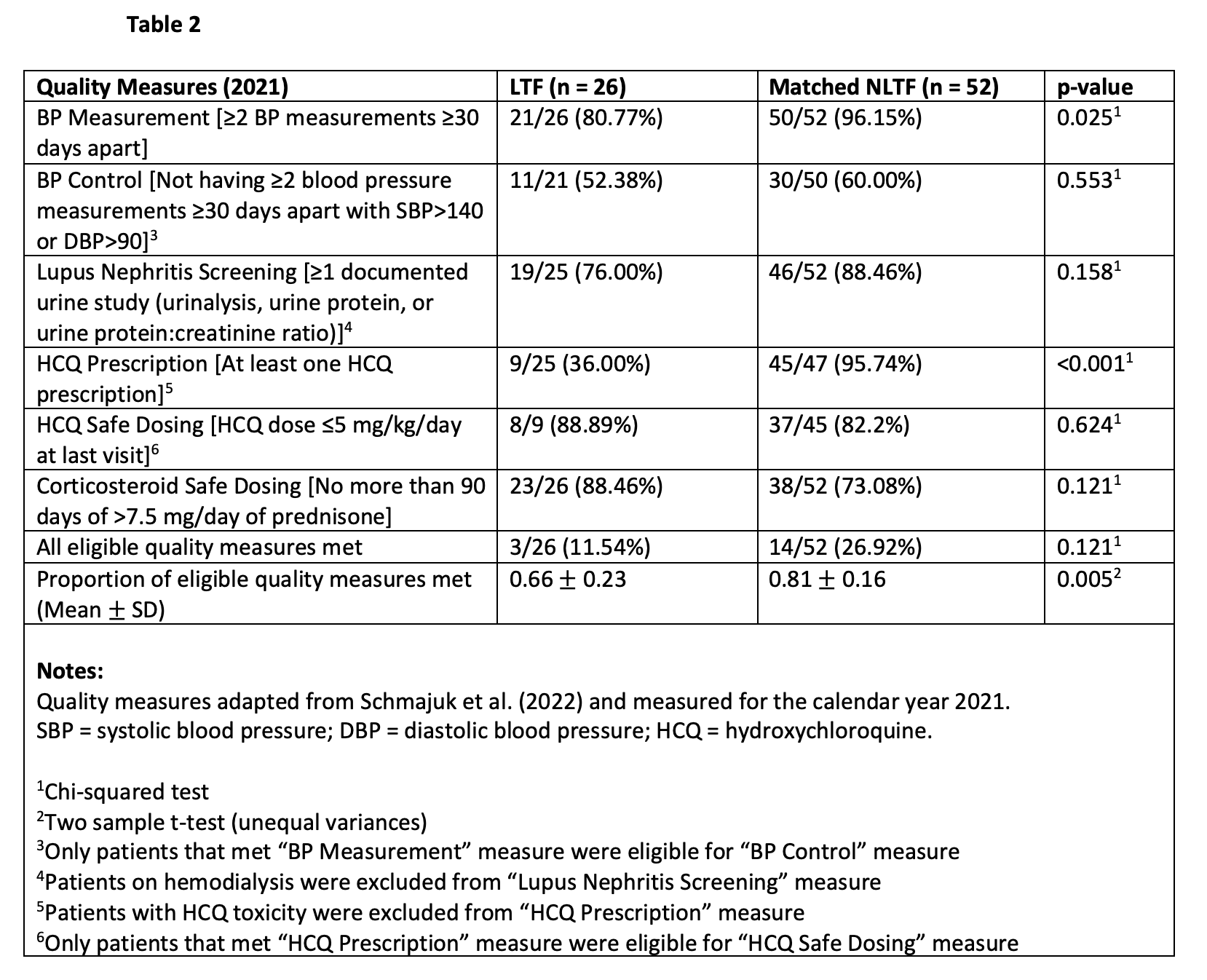
Methods: Using the Lupus Registry at UHB rheumatology clinic, we identified all SLE patients who had any rheumatology visits between 2007 and 2019, excluding patients reported dead in 2021 or earlier. We stratified these patients into three groups based on their follow-up status: lost to follow up (all-LTF; no rheumatology visits in 2020 and 2021), not lost to follow up (all-NLTF; ≥1 rheumatology visits in each year 2019, 2020, and 2021), and inconsistently followed (IF; remaining patients). Within all-LTF, we selected all patients who had ≥2 outpatient visits to UHB at least 30 days apart in 2021 (LTF; n=26). We then matched these patients 1:2 by age and sex to all-NLTF patients with ≥2 outpatient visits to UHB at least 30 days apart in 2021 (NLTF; n=52). Finally, we completed a chart review to identify whether the six SLE quality measures outlined by Schmajuk et al. were met for these patients. To compare LTF and NLTF patients, we used chi-square analyses and a two-sample t-test (α = 0.05).
Results: We determined that of 512 eligible patients in the registry, all of whom satisfied either the 1995 ACR or SLICC criteria for SLE, 265 (52%) were all-LTF and 184 (36%) were all-NLTF [Figure 1]. As expected, the average age (49) and the female prevalence (89%) did not differ between LTF and matched NLTF [Table 1]. Notably, 50% of LTF patients had ESRD (47% with renal transplant), compared to 2% of NLTF patients (2% with renal transplant). NLTF patients received blood pressure measurements and hydroxychloroquine prescriptions at significantly greater rates (96% and 96% respectively) than LTF patients (81% and 36% respectively) [Table 2]. Although not statistically significant, they also tended to receive more urine studies (88%) than LTF patients (76%), but also higher frequency of high dose corticosteroids (27%) than LTF patients (12%). Overall, NLTF patients received a greater proportion of eligible quality measures (0.81) than did LTF patients (0.66).
Conclusion: Only 36% of SLE patients at UHB were consistently followed from 2019-2021. This by itself is an indicator of poor QoC, and may portend poor outcomes. In addition, LTF patients met fewer quality measures than NLTF patients. Conversely, LTF patients tended to have lower corticosteroid doses than NLTF patients, which may be indicative of fewer symptoms, another explanation for their loss to follow up. However, the possibility of subclinical SLE progression, such as lupus nephritis, means that loss to follow up can still be detrimental to these patients. We conclude that loss to follow up is a significant threat to QoC in SLE patients, and that efforts to address follow-up barriers should be made by rheumatologists in collaboration with other health care providers.
To cite this abstract in AMA style:
Kirou R, Avalos C, Ginzler E. Prevalence of Loss to Follow up of Systemic Lupus Erythematosus Patients and Its Effect on Quality of Care [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-loss-to-follow-up-of-systemic-lupus-erythematosus-patients-and-its-effect-on-quality-of-care/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-loss-to-follow-up-of-systemic-lupus-erythematosus-patients-and-its-effect-on-quality-of-care/