Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: While intra-articular (i.a.) mineralization can be visualized on knee radiographs, the sensitivity of its identification is low with this modality, hampering efforts to understand its pathogenic role and consequences in knee OA. Computed tomography (CT) is highly sensitive for the detection and localization of i.a mineralization. We report the prevalence of CT-detected i.a. mineralization in older adults with or at risk of knee OA.
Methods: Bilateral knee CT scans, PA knee radiographs and standard questionnaires to ascertain frequent knee pain are being obtained during the current study visit in the Multicenter Osteoarthritis (MOST) Study, a NIH-funded longitudinal cohort study of persons with or at risk of knee OA. Axial CT images with coronal and sagittal 2D reformats were scored by a musculoskeletal radiologist using an ordinal score (0-3) for degree of mineralization in each of the WORMS subregions of cartilage and meniscus, as well as the soft tissue, capsule, and vasculature. A second MSK radiologist read a random sample of 50 subjects. Prevalence of i.a. mineralization was computed for the total sample, and stratified by age, sex, and presence of frequent knee pain and radiographic knee OA (ROA) (Kellgren and Lawrence grade ≥2).
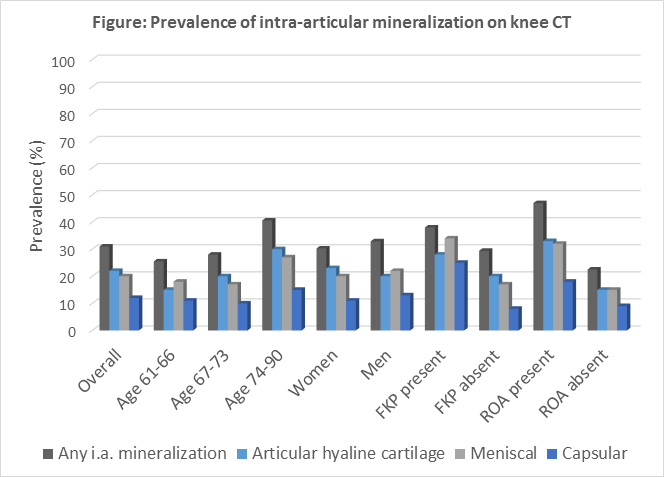
Results: To date, 150 subjects (300 knees) have been scored during the ongoing study visit (53% female, mean age 71, mean BMI 29.8). Overall, 9% of knees had chondrocalcinosis on radiograph, while CT-detected mineralization was present in 31% of knees in cartilage, meniscus, and/or capsule. The prevalence in specific locations was: 22% articular cartilage, 20% meniscal, and 12% capsular (Figure). 24% of knees without chondrocalcinosis on radiograph had articular cartilage and/or meniscal mineralization detected by CT. Of the knees with CT-detected articular cartilage mineralization, the majority had it present in 1-3 WORMS cartilage subregions (out of 14), and 63% also had meniscal mineralization. For the knees with meniscal mineralization, the majority had it in 5 or 6 WORMS meniscus subregions (out of 6), and 60% also had articular cartilage mineralization. Articular and meniscal mineralization increased with age, was similar among men and women, and was more prevalent in those with frequent knee pain and ROA (Figure). Capsular mineralization was similar across age and gender, but more prevalent in those with frequent knee pain and ROA. Overall, 47% of knees had vascular calcification, which increased with age and was more prevalent in men.
Conclusion: CT of the knee provides greater visualization of i.a. mineralization than radiographs, including locations within the hyaline articular cartilage, meniscus, and soft tissue, as well as its co-localization. These data will provide opportunity to evaluate the longitudinal relation of i.a. mineralization to adjacent articular tissue pathology and overall OA progression.
To cite this abstract in AMA style:
Neogi T, Lynch JA, Jarraya M, Clancy MM, Felson DT, Nevitt MC, Lewis CE, Torner J, Guermazi A. Prevalence of Intra-Articular Mineralization on Knee CT in Persons with or at Risk of Knee Osteoarthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-intra-articular-mineralization-on-knee-ct-in-persons-with-or-at-risk-of-knee-osteoarthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-intra-articular-mineralization-on-knee-ct-in-persons-with-or-at-risk-of-knee-osteoarthritis/