Session Information
Date: Friday, November 6, 2020
Title: Epidemiology & Public Health Poster I: COVID-19 & Rheumatic Disease
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Antimalarial drugs (ADs), including chloroquine (CQ) and hydroxychloroquine (HCQ), have anti-inflammatory, immunomodulatory, antiparasitic, anti-thrombotic, and antiviral properties. Their indications in rheumatology have been known for many years, especially in systemic lupus erythematosus, Sjogren’s syndrome, or rheumatoid arthritis. Their recent use in treatment protocols for COVID-19 has been the subject of controversy for a number of reasons, including their potential side effects (SEs). The purpose of this study is to determine the prevalence of SEs, and to study the association between their characteristics and the type of ADs in a rheumatologic population.
Methods: We conducted a retrospective study on medical records of patients hospitalized then followed up in the Department of Rheumatology of the University Hospital of Ibn Rochd, between January 2010 and April 2020, who were treated with CQ or HCQ. The SEs were recorded from a pre-established exploitation sheet. Drug causality was assessed using the World Health Organization Uppsala Medical Center (WHO-UMC) system for standardized case causality assessment. SEs were included if they pertained to the categories of “Certain”, “Probable/Likely”, or “Possible”; and they were excluded if they pertained to the categories of “Unlikely”, “Conditional/Unclassified”, and “Unassessable/Unclassifiable”. The prevalence of SEs is estimated with a confidence interval of 95%, and the study of the factors associated with SEs is performed with univariate analysis with a significance threshold of p < 0.05.
Results: 115 patients received ADs, of which 96% were females, with a mean age of 47 (16 – 82). The indications for ADs were systemic lupus erythematosus (31%), rheumatoid arthritis (30%), and primary Sjogren’s syndrome (18%). The overall prevalence of SEs is 39% (30% – 48%). The specific prevalence of SEs is 37% (26% – 47%) under HCQ, and 45% (28% – 63%) under CQ. 57% of the SEs are ophthalmic, 33% are cutaneous, and 2.2% are cardiovascular. 36% of SEs resulted in the definitive cessation of ADs, 24% under HCQ and 12% under QC. Maculopathy was the main reason for definitive cessation of ADs (43%). The average duration of treatment is significantly different (p < 0.01) with HCQ (3.5 years) versus CQ (7 years). There was no significant association between the categories of SEs and the type of ADs.
Conclusion: In our study, almost two fifths of the patients under ADs presented SEs, with a higher prevalence in the CQ group than in the HCQ group. In addition, prolonged use of ADs is mainly limited by the risk of maculopathy, which is the most frequent cause of definitive cessation. However, the administration of short-course ADs with high doses, as in COVID-19, is likely to modify the prevalence of ADs, compared to those found in rheumatology practice.
 Table 1. Characteristics of the population.
Table 1. Characteristics of the population.
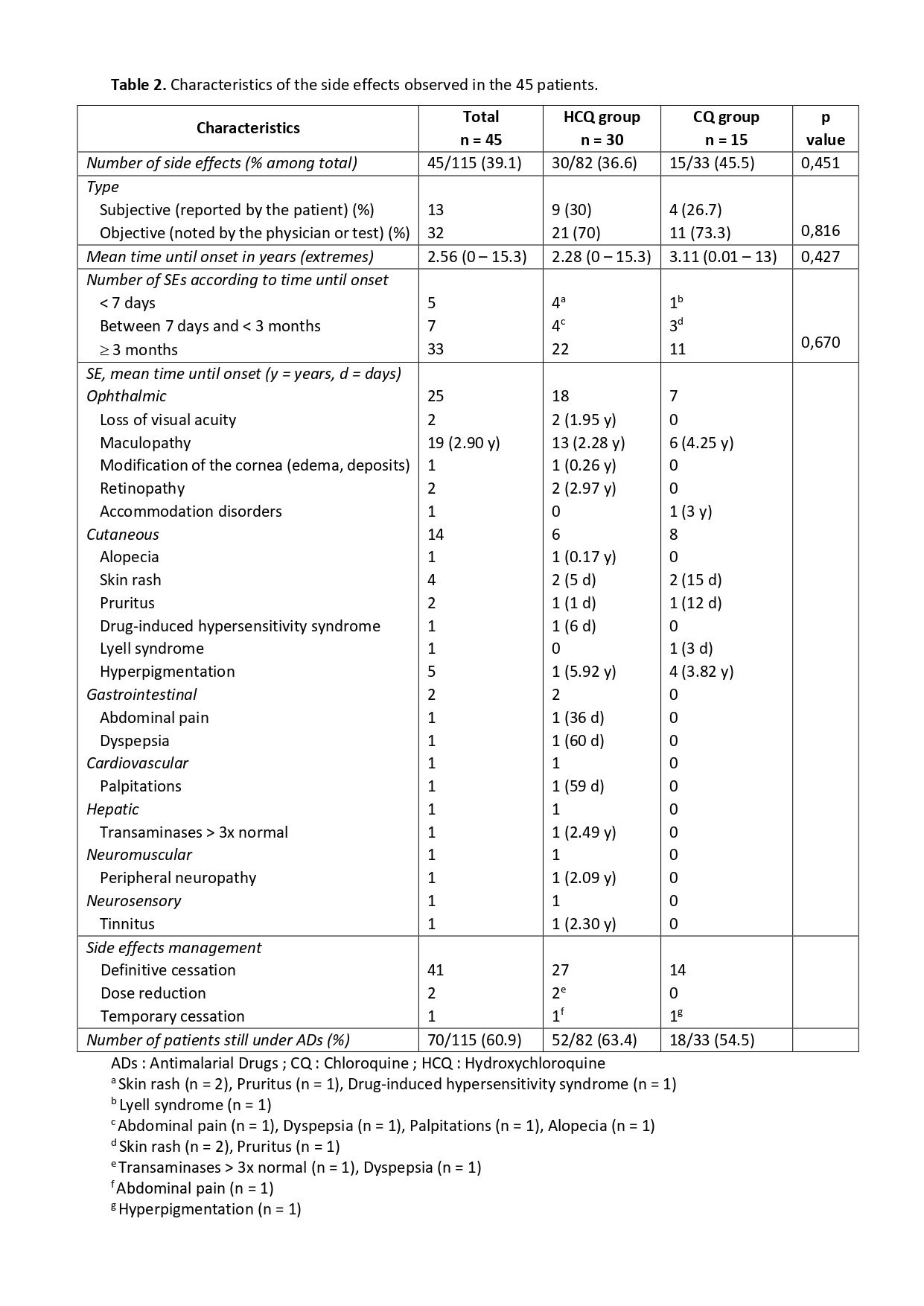 Table 2. Characteristics of the side effects observed in the 45 patients.
Table 2. Characteristics of the side effects observed in the 45 patients.
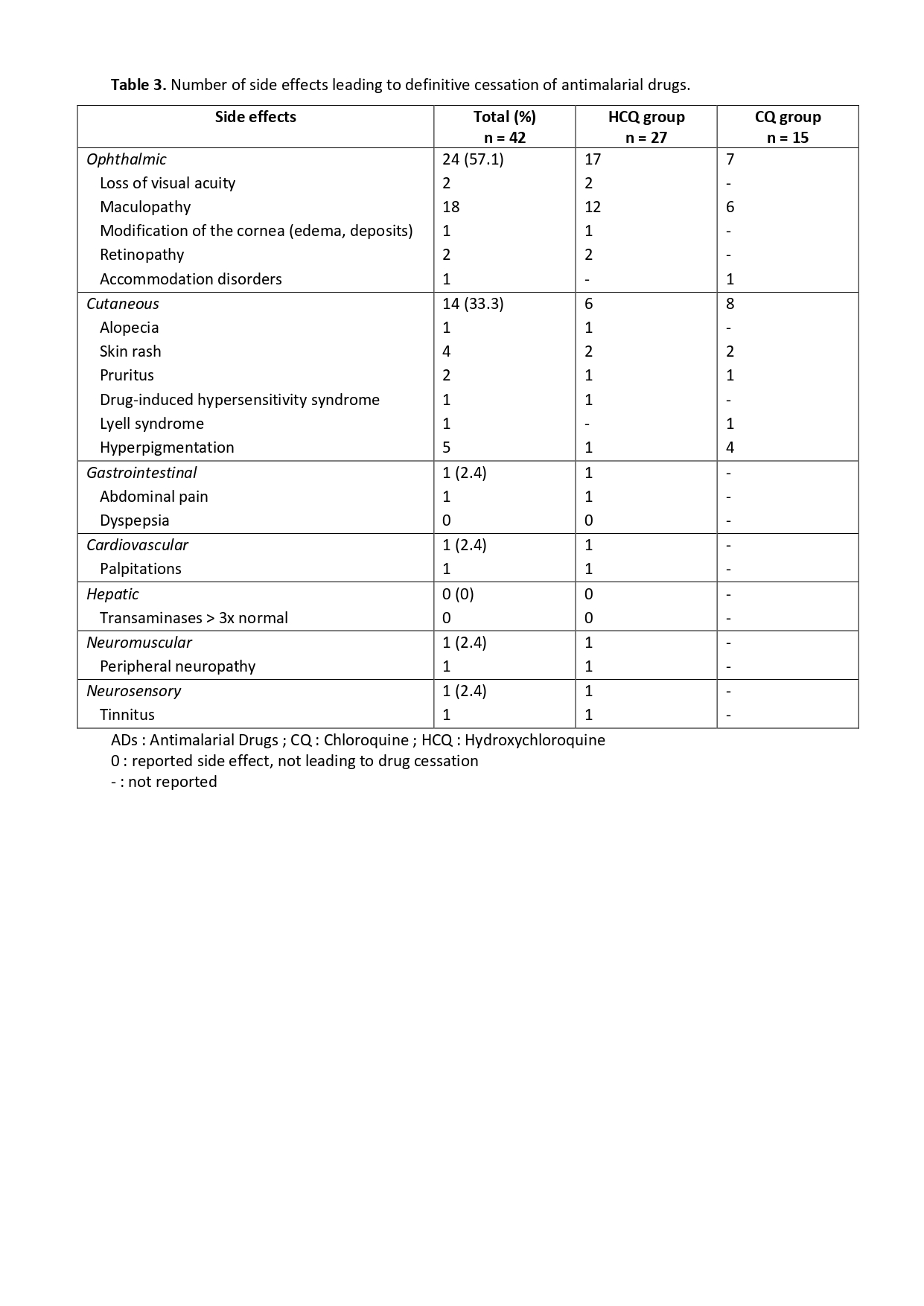 Table 3. Number of side effects leading to definitive cessation of antimalarial drugs.
Table 3. Number of side effects leading to definitive cessation of antimalarial drugs.
To cite this abstract in AMA style:
El Ouali Z, Bassa E, Halidou Idrissa A, Tazi S, Housbane S, Bennani Othmani M, Nassar K, Janani S. Prevalence of Hydroxychloroquine and Chloroquine Side Effects in Rheumatology Patients: A Retrospective Survey of 115 Cases [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-hydroxychloroquine-and-chloroquine-side-effects-in-rheumatology-patients-a-retrospective-survey-of-115-cases/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-hydroxychloroquine-and-chloroquine-side-effects-in-rheumatology-patients-a-retrospective-survey-of-115-cases/
