Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) are known to have hepatic injury (HI), however large-scale longitudinal studies are lacking.We report our experience of HI in SLE patients.
Methods: A retrospective longitudinal single center study was conducted from 1994-2022 to identify patients enrolled in natural history protocol for SLE. Inclusion: 1) Age ≥ 18 years; 2) Diagnosis of SLE based on 1997 American College of Rheumatology revised criteria. Exclusion: Patients with either < 3 visits or < 6 months of follow-up. Demographic, laboratory, medication and liver histology data (when available) were obtained from the electronic medical records. Patients were divided into two categories- with and without HI. HI was divided into 5 categories- persistent hepatocellular injury, transient hepatocellular injury, persistent cholestatic injury, transient cholestatic injury and mixed. Patients were allowed to be in more than one category. Chi-square test and Kruskal-Wallis tests were used for comparing categorical and numerical variables, respectively. P-value < 0.05 was considered statistically significant and R software was used for all statistical analyses.
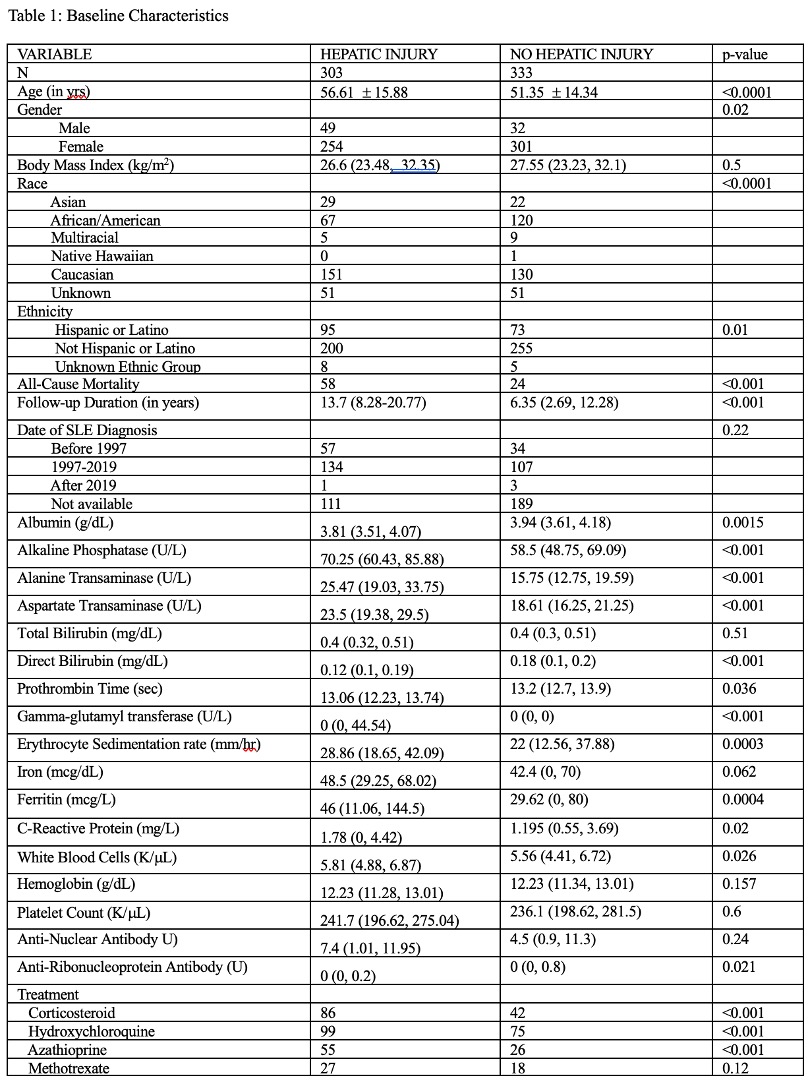
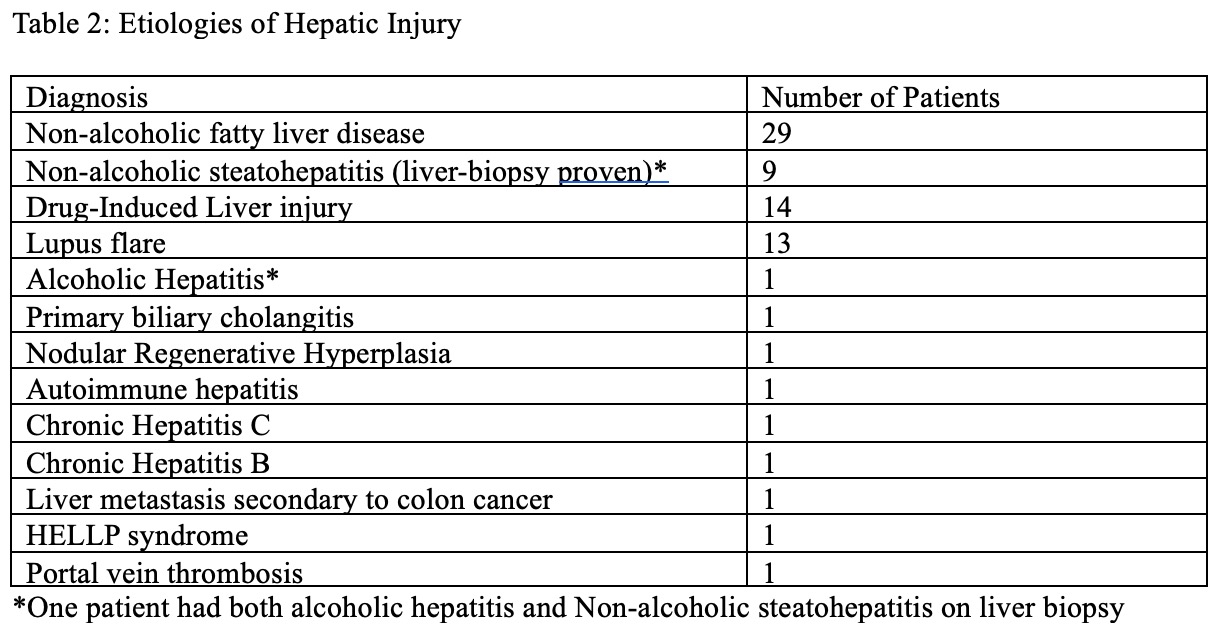
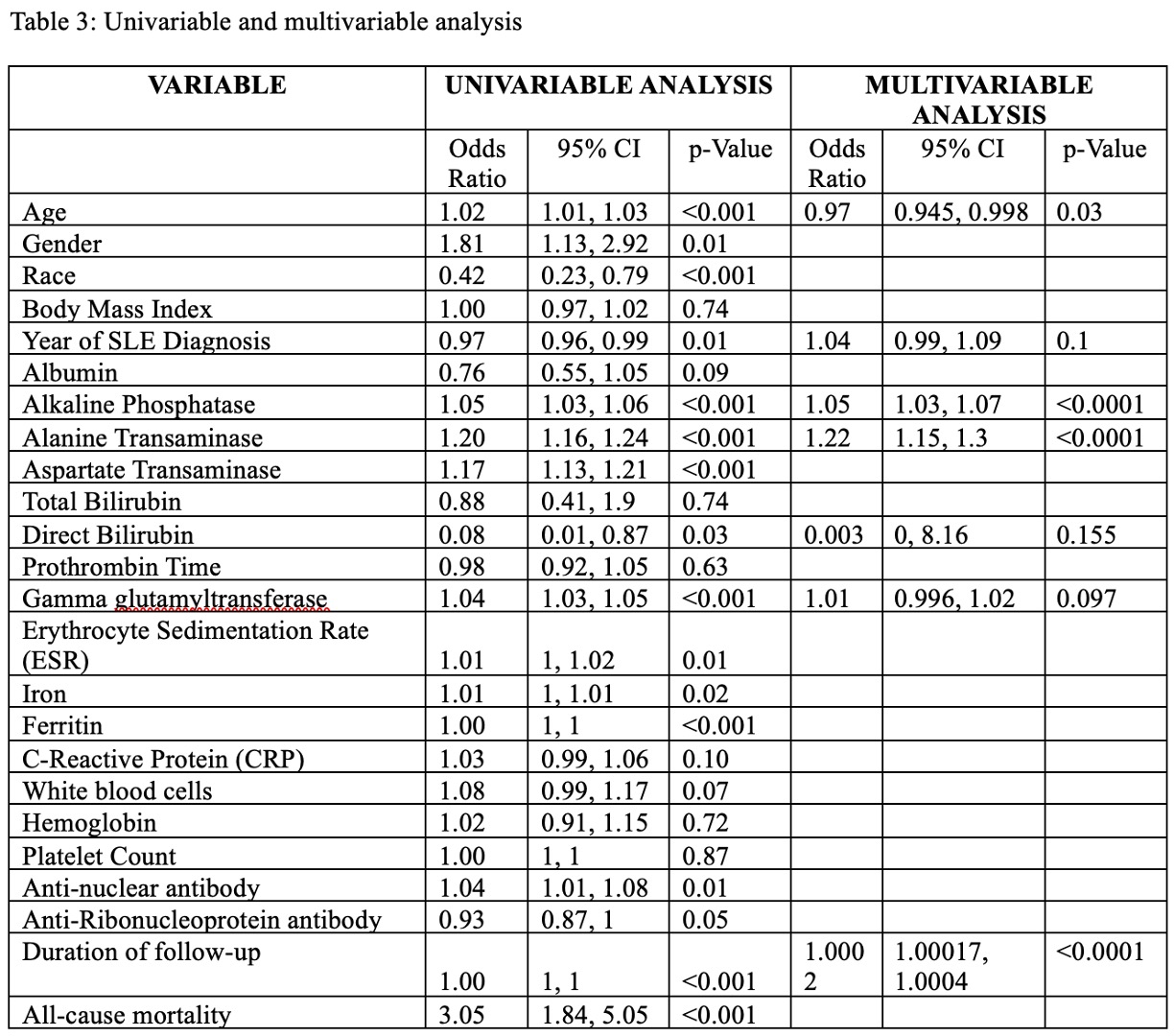
Results: Out of 1106 patients, 636 patients were included in the final cohort, with median duration of follow-up of 9.7 yrs (IQR 4.15-16.96). Mean age was 53.85 yrs (±15.31) and majority were females (555, 87.26%). A large proportion of patients (303, 47.64%) developed HI- persistent hepatocellular injury, transient hepatocellular injury, persistent cholestatic injury, transient cholestatic injury and mixed injury were present in 91, 174, 55, 78 and 67 patients, respectively. Patients with HI were older, more likely to be male, Asian, Caucasian or Hispanic and less likely to be African American (Table 1). Patients with HI also had longer follow-up. In majority of patients (230, 75.91%), the cause of HI could not be identified. Of the remaining 73 patients, non-alcoholic fatty liver disease was the most common, followed by drug-induced liver injury, SLE flare and non-alcoholic steatohepatitis (Table 2). On univariable analysis, apart from liver enzymes, age, gender, race, date of SLE diagnosis, duration of follow-up, iron, ferritin, ESR, and ANA were significantly associated with HI (Table 3). However, on multivariable analysis, only alkaline phosphatase, alanine transaminase and duration of follow-up remained associated with higher odds of HI, while older age was associated with lower odds, suggesting patients tend to develop HI at a younger age. All-cause mortality was higher in patients with HI.
Conclusion: A large number of SLE patients develop HI during the course of the disease, with transient hepatocellular injury the most common type of HI. While males and Asians, Caucasians and Hispanics seem to be at a higher risk, African-Americans seem to be at lower risk of HI, although in a majority of patients the cause remains unclear. Fatty liver disease was the most common cause of liver disease, although patients were also found to have autoimmune hepatitis, primary biliary cholangitis and nodular regenerative hyperplasia. Higher mortality in patients with liver disease might suggest a more severe SLE disease course and consequently worse outcomes.
To cite this abstract in AMA style:
Hitawala A, Manna Z, Temesgen-Oyelakin Y, Poncio E, Koh C, Hasni s, Heller T. Prevalence of Hepatic Injury in Patients with Systemic Lupus Erythematosus: A 28-Year Single Center Experience [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-hepatic-injury-in-patients-with-systemic-lupus-erythematosus-a-28-year-single-center-experience/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-hepatic-injury-in-patients-with-systemic-lupus-erythematosus-a-28-year-single-center-experience/