Session Information
Date: Monday, November 13, 2023
Title: (1264–1307) RA – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Studies have demonstrated a link between frailty and chronic inflammation, raising the question of whether chronic inflammatory diseases like rheumatoid arthritis (RA) may be associated with increased rates of frailty. Our objective was to evaluate the prevalence of frailty among individuals living with RA compared to the general population without RA.
Methods: We conducted a population-based cohort study using administrative health data for a Canadian province from 1990 – 2018. A previously validated case definition based on physician billing data was used to assemble an incident cohort of all cases with RA onset from 1996 – 2008. To capture the health state of individuals living with RA, the baseline date was defined as 5 years after the index date for RA diagnosis. A random sample of 50% of incident RA cases was included in this analysis, none of which were used for the derivation of our frailty measure. Each RA individual was matched 2:1 by sex, birth year, and index year with randomly selected individuals from the general population with no physician visits for any type of inflammatory arthritis. For controls, the index date was defined as the date of a randomly selected health care encounter occurring in the same calendar year as the index year of the RA case to which they were matched, and the baseline date was defined as 5 years after this index date. Frailty was measured using a frailty index (FI), which we previously developed using a combination of data-driven and consensus-based methods. The FI includes 40 health deficits, the presence of which was evaluated using administrative health data for the 3 years prior to the baseline date. Each deficit was scored from 0 (absent) to 1 (present) and individual deficit scores were summed and divided by the total number of deficits to produce a baseline FI score for each individual. Frailty was defined as a baseline FI score > 0.21. We compared the prevalence of frailty among RA patients and non-RA controls using conditional logistic regression. The number of health deficits present was compared between RA patients and non-RA controls using negative binomial regression. Multivariable models were stratified by age, sex, and calendar year, and were adjusted for rurality, socioeconomic status, and baseline scores for the Romano version of the Charlson comorbidity index (CCI).
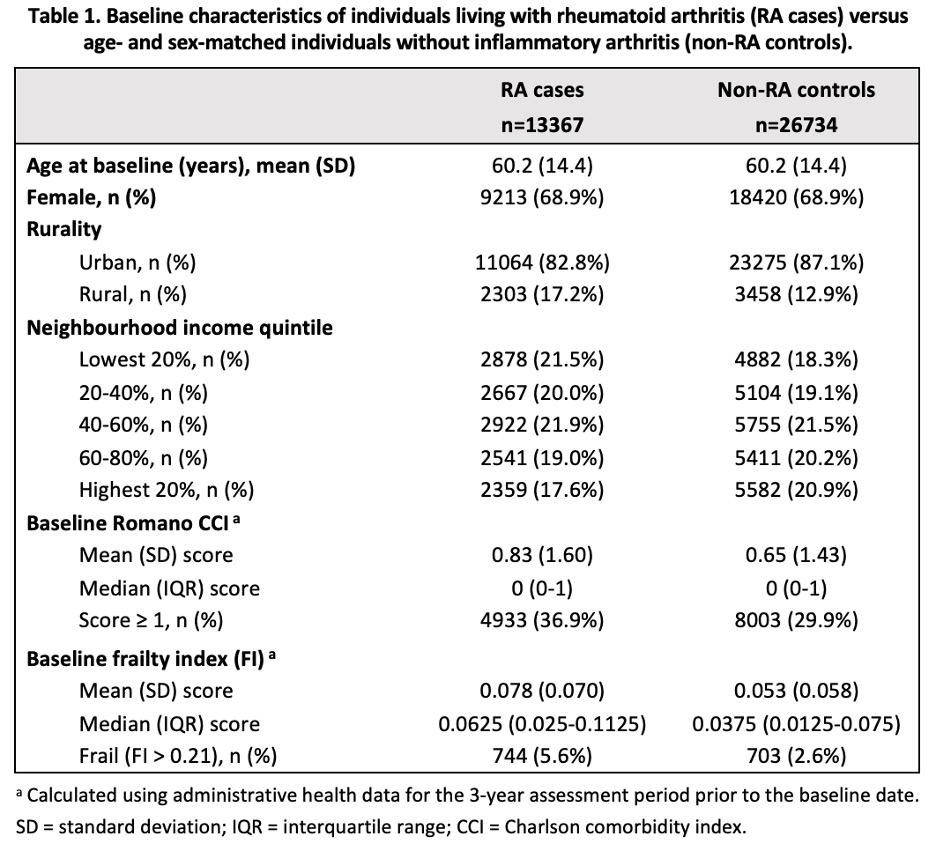
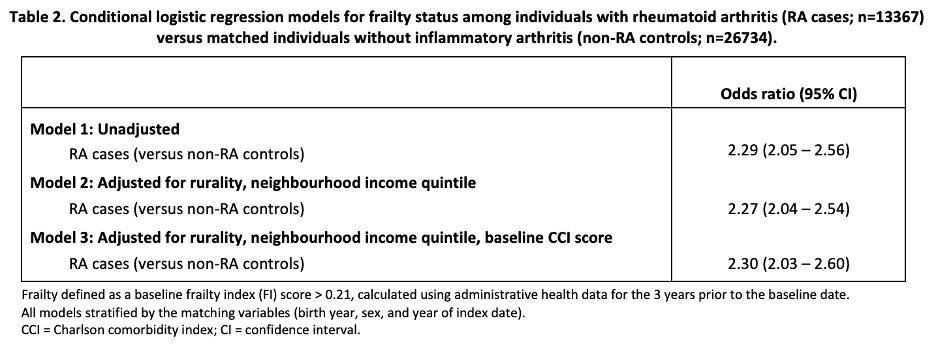
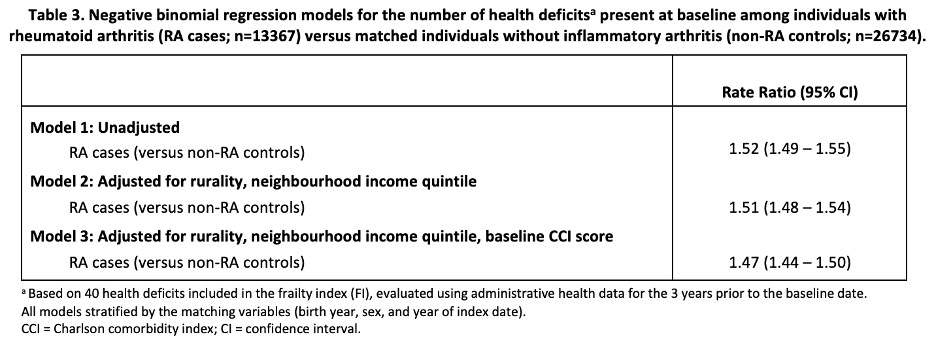
Results: Baseline characteristics for RA patients (n=13367) and non-RA controls (n=26734) are shown in Table 1. Baseline FI scores were significantly higher among RA patients compared to non-RA controls and a greater proportion of RA patients were considered frail at baseline (Table 1). The odds of frailty were significantly higher among RA patients compared to non-RA controls, and this relationship was unchanged following adjustment for potential confounders (Table 2). Similar results were obtained for the number of health deficits present at baseline (Table 3).
Conclusion: Frailty is significantly more common among individuals living with RA when compared to age- and sex-matched individuals without inflammatory arthritis. Future work will aim to better understand the reasons for these differences and identify strategies to prevent and treat frailty in RA.
To cite this abstract in AMA style:
Legge A, Lacaille D. Prevalence of Frailty Among Individuals Living with Rheumatoid Arthritis: A Population-based Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-frailty-among-individuals-living-with-rheumatoid-arthritis-a-population-based-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-frailty-among-individuals-living-with-rheumatoid-arthritis-a-population-based-cohort-study/