Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Increased risk of cervical dysplasia and cervical cancer have been reported in patients with systemic lupus erythematosus (SLE). However, the reason for this increased risk is not known but may be related to chronic inflammation or immunosuppressive medications. We hypothesize that patients with Antisynthetase Syndrome (ASS), which is also an inflammatory disease treated with immunosuppression, will have an increased risk of cervical abnormalities. There has not previously been a study evaluating the risk of cervical dysplasia or cervical cancer in ASS patients.
Methods: Clinical data were obtained by retrospective review of EMR at Cleveland Clinic (CC) from 2000-2020. Female patients, over the age of eighteen, diagnosed with ASS by a CC rheumatologist and with the presence of one of the ASS specific autoantibodies (Ab): Jo-1, PL-7, PL-12, EJ, or OJ, were selected. Patients with SLE diagnosed by a CC rheumatologist were age-matched to the ASS patient cohort. An age-matched control population without any known autoimmune rheumatic disease was obtained through the Medicine Institute Value-Based Care Research Registry. In addition to the above criteria, the patients were also required to have Pap smear data available in the EMR. Patients who carried concurrent diagnoses of ASS and SLE were excluded from the study.
Results: A total of 135 patients were included in our analysis with 45 patients in each subgroup: ASS, SLE, or controls. The median age was 52 years. Cervical abnormalities, including cervical inflammation, cervical dysplasia, and cervical cancer, were compared between groups. More than half (53.3%) of all patients had some degree of cervical abnormality, most commonly cervical inflammation (27/74, 37%) and atypical squamous cells of undetermined significance (ASCUS) (27/74, 37%). There were no statistically significant differences in the presence of cervical abnormalities between the three groups. Cervical cancer was present in 6 patients. HPV infections were documented in 23% of patients (31/135), and even after multivariable analysis HPV remained a strong predictor of cervical abnormalities (p= < 0.001). There was also a trend towards use of oral contraceptive pills (OCPs) predicting cervical abnormalities, but this did not reach statistical significance once multivariable logistic regression was completed (p=0.054).
Conclusion: In our cohort, there was no statistically significant difference in the prevalence of cervical dysplasia and cervical cancer in the three groups. This is an interesting finding as numerous studies have reported an increased prevalence of cervical abnormalities in SLE patients, but this was not found in our cohort. The reason for this is unclear but may be related to the small number of ASS patients available for review. Additionally, there may be selection bias towards sicker patients who are more likely to be encouraged to have age-appropriate cancer screening. Our study was limited by being a single-center retrospective analysis of a relatively small cohort. Further studies, with larger sample sizes, maybe helpful to fully understand the underlying risk factors contributing to the prevalence of HPV, cervical dysplasia, and cervical cancer in SLE and ASS patients.
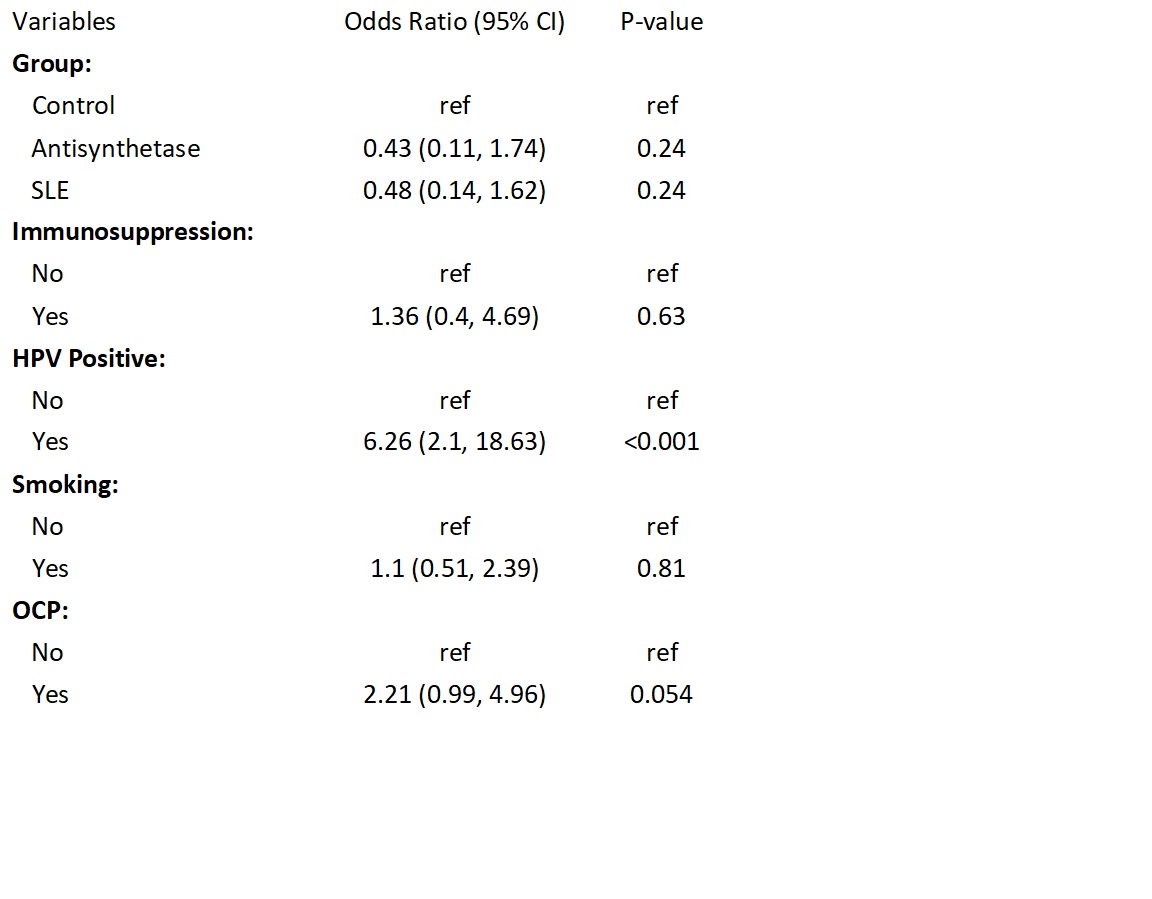 Table 1: Multivariable Logistic Regression
Table 1: Multivariable Logistic Regression
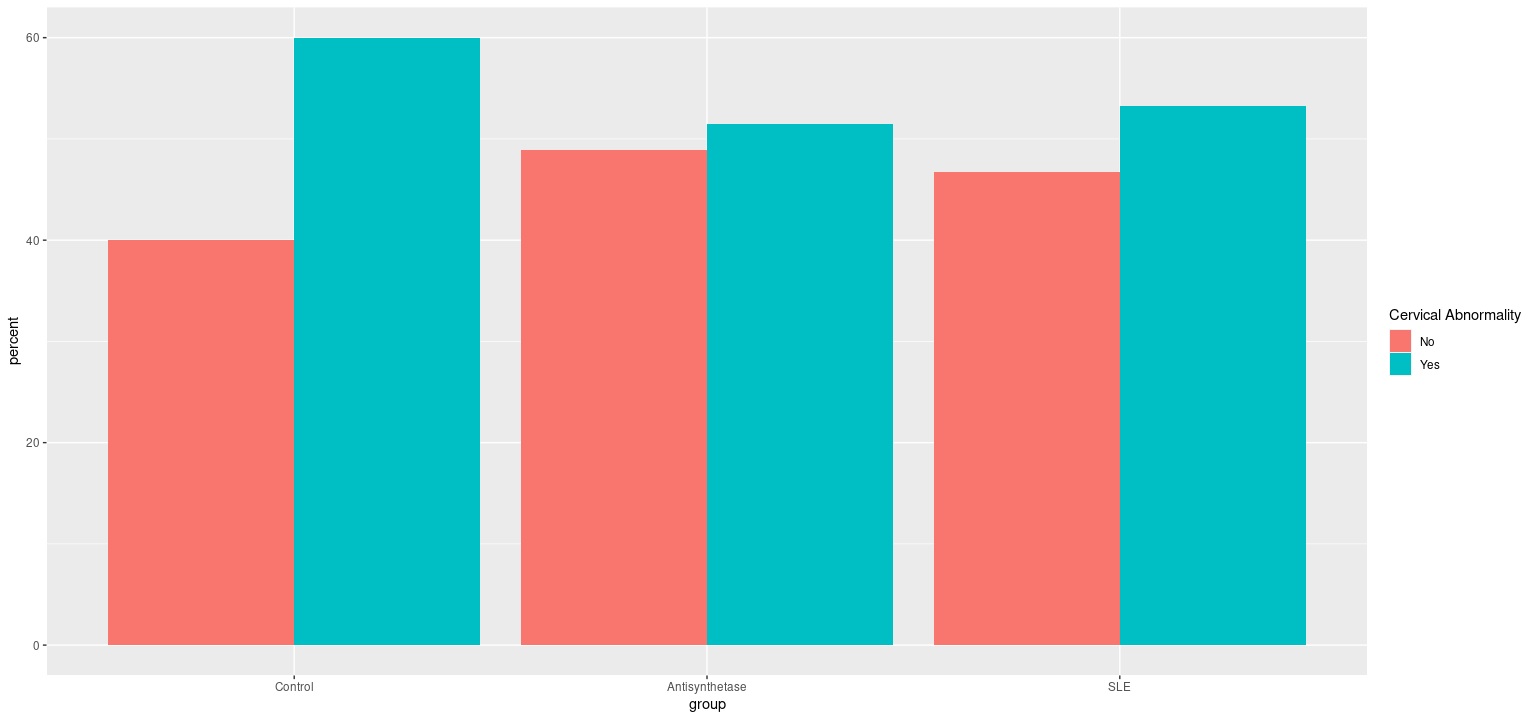 Figure 1: Comparison of the Presence of Cervical Abnormalities by Group
Figure 1: Comparison of the Presence of Cervical Abnormalities by Group
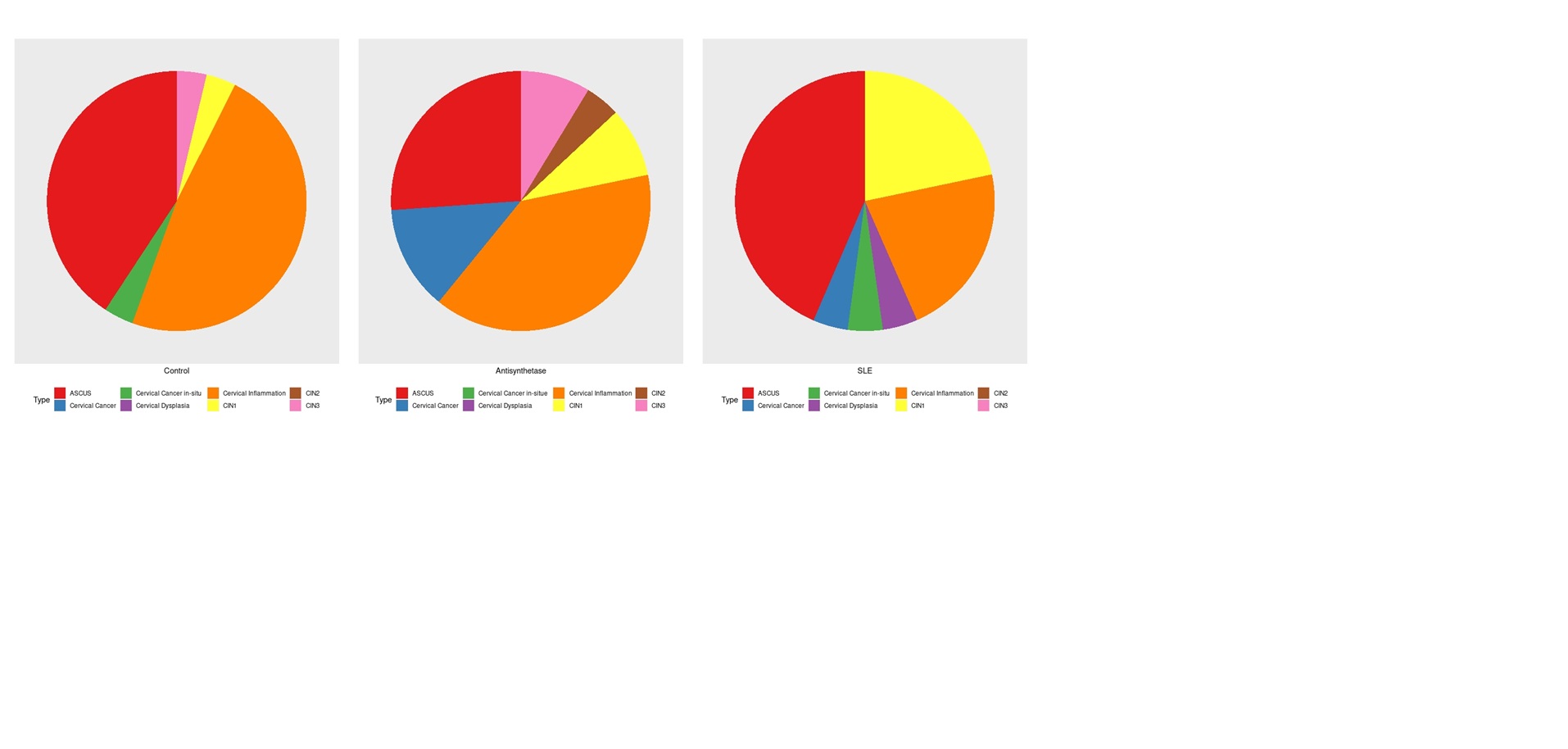 Figure 2: Comparison of Cervical Abnormality Type by Group
Figure 2: Comparison of Cervical Abnormality Type by Group
To cite this abstract in AMA style:
Katz A, Jin Y, Chatterjee S. Prevalence of Cervical Dysplasia in Women with Antisynthetase Syndrome [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/prevalence-of-cervical-dysplasia-in-women-with-antisynthetase-syndrome/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-cervical-dysplasia-in-women-with-antisynthetase-syndrome/
