Session Information
Date: Monday, November 13, 2023
Title: (1442–1487) SLE – Diagnosis, Manifestations, & Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with SLE are at increased risk for cardiovascular disease (CVD). Population estimates of CVD in SLE remains limited for non-White racial/ethnic populations in the United States. The Manhattan Lupus Surveillance Program (MLSP), a population-based retrospective registry of SLE patients, was used to investigate the prevalence of CVD among SLE patients in 2007.
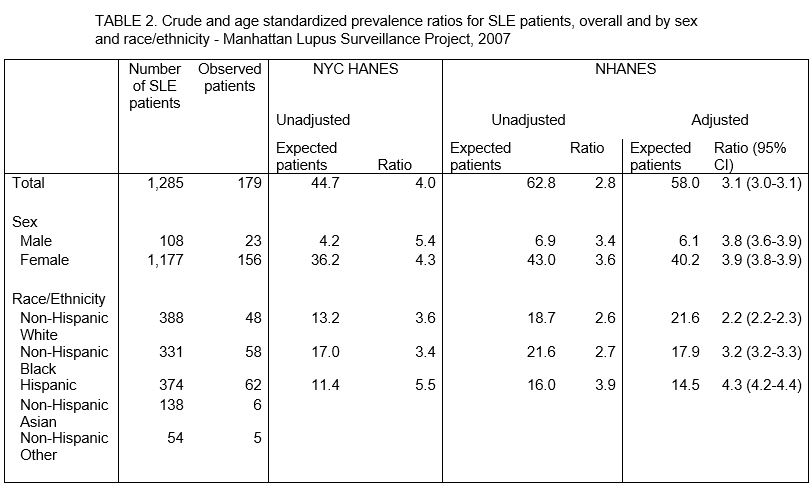
Methods: MLSP patients were identified from rheumatologists, hospitals and population databases using ICD-9 codes. We included prevalent SLE patients aged ≥20 residing in Manhattan in 2007 who met one of the SLE classification criteria: 1997 ACR, SLICC or EULAR/ACR. CVD was captured if documentation existed confirming a myocardial infarction (MI) or cerebrovascular accident (CVA). Crude risk ratios were calculated for sex, age group, and race/ethnicity, and adjusted risk ratios (ARR) controlled for sex, age group, race/ethnicity and number of years since diagnosis. We used data from the National Health and Nutrition Examination Survey (NHANES 2009–2010) and the NYC Health and Nutrition Examination Survey (NYC HANES 2013–2014) to determine the prevalence of MI or CVA nationally and in NYC, respectively. Estimates for those identified as non-Hispanic Asian and non-Hispanic other race/ethnicity were not included, as they were either not available (NHANES) or estimates were unreliable (NYC HANES). We calculated the expected prevalence of MI or CVA by multiplying NHANES and NYC HANES prevalence estimates by strata-specific counts of MLSP SLE patients. We calculated crude prevalence ratios using both national and NYC estimates and age standardized prevalence ratios (ASPR) with three age groups using national estimates. We were unable to calculate age standardized prevalence ratios using the NYC estimates, as prevalence estimates broken down by demographic group and age group were unreliable.
Results: Overall 1285 patients met SLE classification criteria (92% female, 30% non-Hispanic White, 26% non-Hispanic Black, 29% Hispanic, 11% non-Hispanic Asian.) CVD occurred in 179 (13.9%), occurred less frequently among women (ARR 0.6, 95% CI 0.4-0.8), and risk increased with age, Table 1. Compared with non-Hispanic White patients, risk of CVD was elevated among non-Hispanic Black (ARR: 1.8, 95%CI 1.3-2.6) and Hispanic SLE patients (ARR: 1.6 ,95%CI 1.1-2.3), Table 1. CVD prevalence was approximately 3 times higher among MLSP patients than national estimates (ASPR: 3.1,9 5%CI 3.0-3.1) and ASPRs did not differ by sex, Table 2. Compared with the national population, the ASPR among SLE patients was most elevated among Hispanics (4.3, 95% CI 4.2-4.4) followed by non-Hispanic Blacks (3.2, 95% CI 3.2-3.3) and non-Hispanic Whites (2.2, 95% CI 2.2-2.3), Table 2. Unadjusted prevalence ratios of CVD were also elevated in comparison with NYC residents (4.0), particularly among men (5.4) and Hispanics (5.5).
Conclusion: These findings provide population-based estimates of CVD amongst a multi-racial/ethnic SLE registry These data can help providers ensure SLE patients are appropriately screened for CVD disease.
Patients include residents of Manhattan in 2007 with a new or existing diagnosis of SLE by ACR, EULAR, or SLICC criteria who are aged 20 or older.
*Adjusted risk ratios were calculated from a Poisson model which incorporated sex, age group, race/ethnicity, and years since SLE diagnosis. 41 patients were excluded due to missing race/ethnicity information.
To cite this abstract in AMA style:
Joyce D, Berger J, Guttmann A, Hasan G, Buyon J, Belmont H, Salmon J, Askanase A, Bathon J, Geraldino-Pardilla L, Ali Y, Ginzler E, Putterman C, Gordon C, Helmick C, Barbour K, Gold H, Parton H, Izmirly P. Prevalence of Cardiovascular Disease in a Populations Based Registry of Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-cardiovascular-disease-in-a-populations-based-registry-of-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-cardiovascular-disease-in-a-populations-based-registry-of-patients-with-systemic-lupus-erythematosus/