Session Information
Date: Sunday, November 12, 2023
Title: (0609–0672) Systemic Sclerosis & Related Disorders – Clinical Poster I: Research
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Gastrointestinal manifestations of systemic sclerosis are common and include luminal dysmotility. Esophageal aperistalsis (scleroderma esophagus) presents with dysphagia and reflux; and can predispose patients to esophagitis, theoretically increasing the risk for Barrett’s esophagus, which is a known risk factor of esophageal adenocarcinoma. However, no current data is available in literature regarding the risk of Barrett’s esophagus or esophageal adenocarcinoma in patients with SS.
Methods: A retrospective cohort study was conducted using the multi-institutional research network TriNetX. All patients with systemic sclerosis (age 16 and above) were identified. Prevalence and incidence proportion of Barrett’s esophagus were calculated for the year 2022.
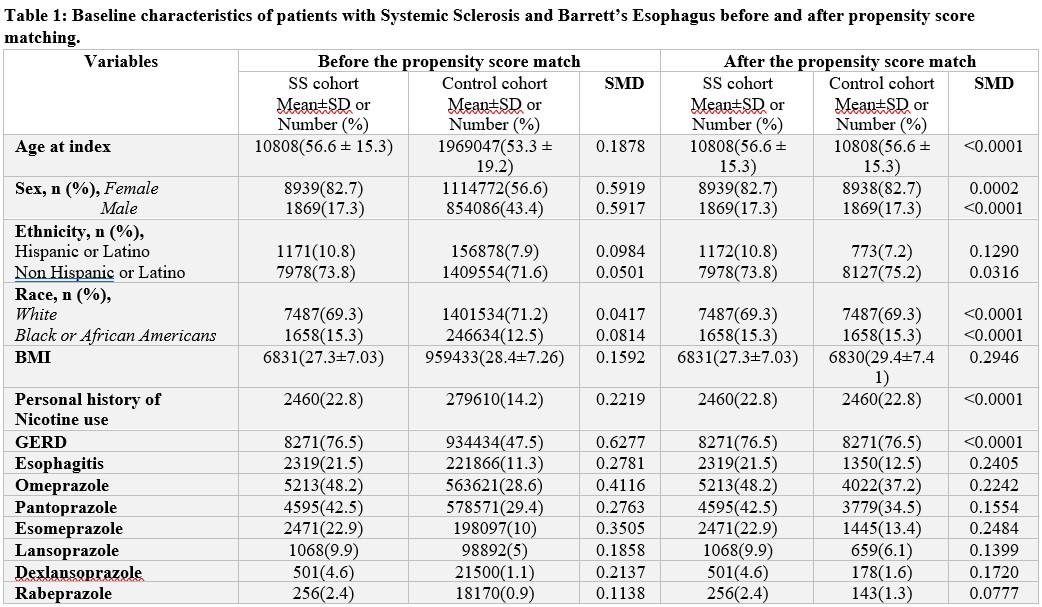
Propensity matched analysis was then performed, utilizing age, gender, race, presence of GERD, and history of smoking as covariates, to compare rates of BE diagnosis at index endoscopy in patients with and without SS who underwent EGD during the study time period.
Results: A total of 60,907 patients with SS were identified in the research network. The prevalence and incidence proportion of Barrett’s esophagus in patients with SS during 2022 were calculated to be 3.96% and 0.39% respectively. Incidence rate of BE diagnosis in the cohort was 0.000014 cases/ person day. The prevalence and incidence rate of Barrett’s esophagus in patients without SS during the same period was 0.54% and 0.074% respectively.
Patients with SS who underwent EGD examinations were identified and 1:1 propensity score matching was performed to identify a control cohort of patients without SS who underwent index EGD during the study period (10,808 patients in each cohort). In PSM analysis, the risk of Barrett’s esophagus diagnosis at index esophagogastroduodenoscopy (EGD) was not different between patients with systemic sclerosis compared to patients without SS who underwent EGD for any indication [3.67% vs 3.37 %, RR: 1.09 (0.95 – 1.25)]. However, the risk of BE esophagus diagnosis at any time during follow up was higher in patients with SS [8.11% vs 6.17%, RR: 1.32 (1.19-1.45)]. No difference was noted in rates of esophageal cancer diagnosis in the two cohorts [0.86% vs 0.96%, RR: 0.89 (0.68-1.18)].
Conclusion: The prevalence and incidence rate of BE diagnosis in patients with SS is high. Provider vigilance is advised, and EGD screening and proton pump inhibitor therapy should be considered in patients with SS with upper GI symptoms.
To cite this abstract in AMA style:
Rida Ul Jannat F, Verma D, Sakkal L. Prevalence of Barrett’s Esophagus in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-of-barretts-esophagus-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-of-barretts-esophagus-in-patients-with-systemic-sclerosis/