Session Information
Date: Sunday, November 7, 2021
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatoid arthritis (RA) patients have a higher risk of developing infections as compared to the patients without the diagnosis, and this risk is further augmented by the use of biologics and immunosuppressant medications used for the treatment. This could be explained by the disease process itself, associated comorbidities, and immunomodulation as a result of the treatment modalities. We aim to identify national trends in terms of the common infectious etiologies in RA patients leading to hospitalizations in the patients admitted within a 15 year time period.
Methods: We used the Nationwide Inpatient Sample (NIS) database (years 1999-2014) and extracted all patients with Rheumatoid Arthritis using validated International Classification of Disease (ICD) codes. Further, six common hospitalized infections were identified: Urinary tract infection (UTI), Pneumonia, Skin and soft tissue infection (SSTI), Sepsis, Bacteremia, and Opportunistic infections. Data was analyzed using Statistical Analysis System (SAS) 9.4 software.
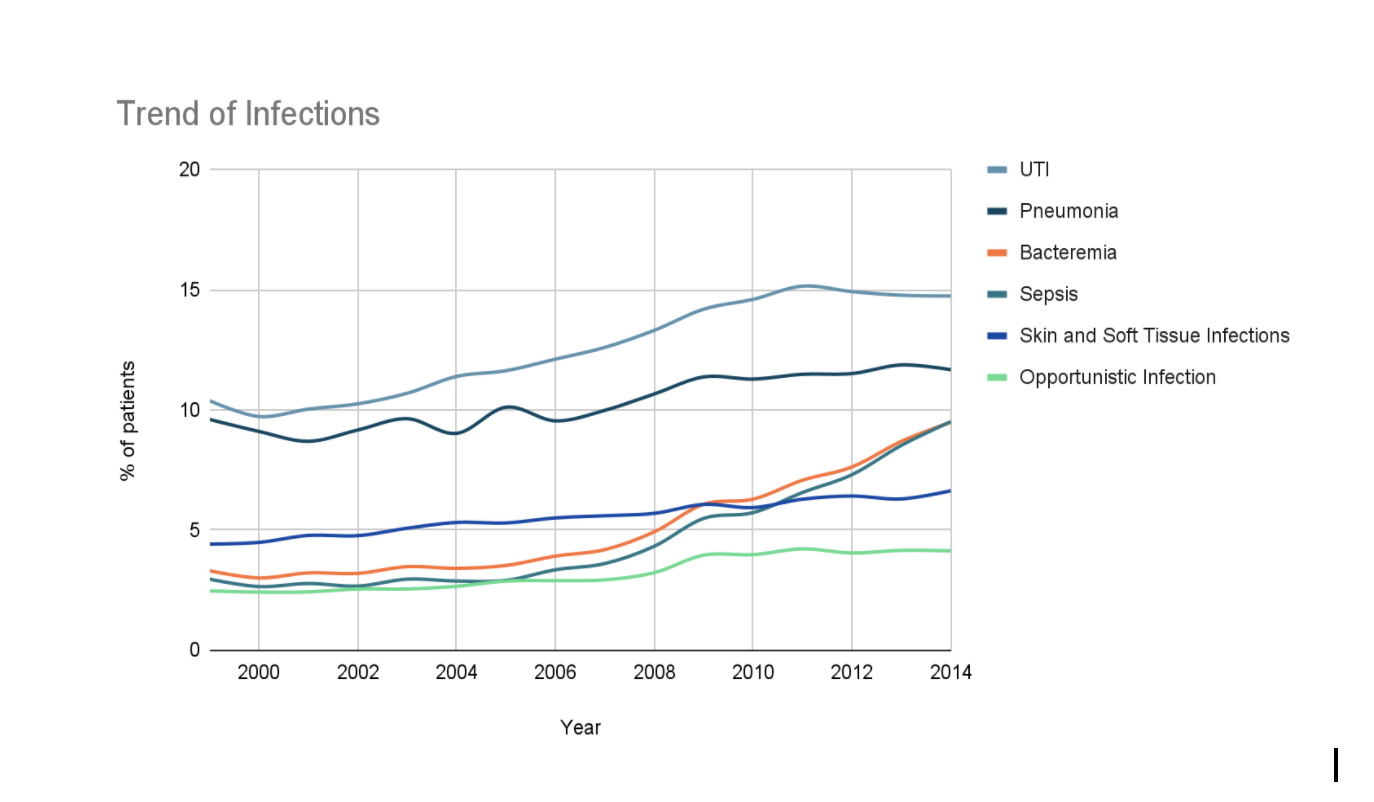
Results: A total of 1,351,284 cases of Rheumatoid arthritis were identified in the 15 year period (1999-2014). Mean age was 66.55 ± 15.34 years with females making up 74.95% (n= 1,012,532) of the patient population. As seen in Figure 1, an overall upward trend was noticed in all 6 selected infections (p< 0.001). It was found that UTI was the most prevalent infection in this population, which was on the rise from 10.38% in 1999 to 15.15% in 2011, with a steady decline to 14.74% in 2014, followed by Pneumonia (9.6% in 1999, 11.67% in 2014). Sepsis (3.34% in 2006 to 9.51% in 2014) and Bacteremia (3.91% in 2006 to 9.48% in 2014) had a dramatic increase since 2006.
Length of stay (LOS) in RA patients without any infection is 4.43 days and the average cost is $29,833.65 whereas in RA patients with any of the infections, LOS increases to 6.95 days and the average cost is $39,214.49.
Conclusion: The use of biological agents for the treatment of RA is associated with improved outcomes by decreasing inflammation and improving the overall mortality and morbidity in RA patients. However, at the same time, this has led to a higher rate of infections as a result of immune suppression in RA patients. It has been reported that tumor necrosis (TNF) inhibitors are associated with a higher rate of infection when compared to conventional disease modifying agents, especially UTI, pneumonia and SSTI. In our study, we noticed that the common infections in hospitalized patients with RA included UTI and Pneumonia, both of which have risen since 1999. Higher UTI prevalence can also be explained by the female predominance. An increase in Sepsis was also seen which could be attributed to a higher infection rate, but maybe overestimated or correctly estimated as compared to past secondary to better coding and documentation of sepsis. Higher infection rates also contributed to longer hospital stays, thus leading to higher costs of care in these patients. Thus, there needs to be increased infection surveillance in this patient population, especially with the increasing use of biologic agents.
To cite this abstract in AMA style:
Khandwala P, Hussain A, Desai D. Prevalence and Trends of Infections in Hospitalized Patients with Rheumatoid Arthritis in the United States [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-trends-of-infections-in-hospitalized-patients-with-rheumatoid-arthritis-in-the-united-states/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-trends-of-infections-in-hospitalized-patients-with-rheumatoid-arthritis-in-the-united-states/