Session Information
Date: Monday, November 18, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with psoriatic disease (PsD) [psoriasis (PsO) and psoriatic arthritis (PsA)] are at greater risk of developing metabolic dysfunction-associated steatotic liver disease (MASLD) compared with the general population. In addition, PsD has a more severe progression of MASLD and it is associated with an increased risk of cardiovascular disease and its consequences.
OBJECTIVES: To assess the prevalence of MASLD and the degree of fibrosis in our PsD population compared to a group of healthy volunteers. A second aim was to determine the prevalence of cardiovascular risk factors in the PsO and PsA groups.
Methods: Cross-sectional study from a single centre in which 207 consecutive patients from the departments of Dermatology and Rheumatology were included. Patients with any severity or duration of inflammatory disease were included. None of the patients enrolled had a history of known liver disease. Then 102 healthy people (without any chronic inflammatory disease or liver disease) were recruited.
Body weight, height and general patient assessment were recorded. Blood samples were extracted and FibroScan® technology was used, a validated transient elastography method. We assessed the Fibrosis score (kPA) that measures liver stiffness (pathological ≥F2) and the controlled attenuation parameter dB/m (CAP) score that assesses steatosis (pathological ≥S1). Baseline demographics (age, sex, BMI, dyslipidaemia, hypertension and diabetes status), biochemistry (blood glucose, HOMA, transaminases (ALT and AST), LDL-cholesterol, HDL-cholesterol and triglycerides) and FibroScan results (steatosis and fibrosis) were compared between PsD patients and healthy subjects.
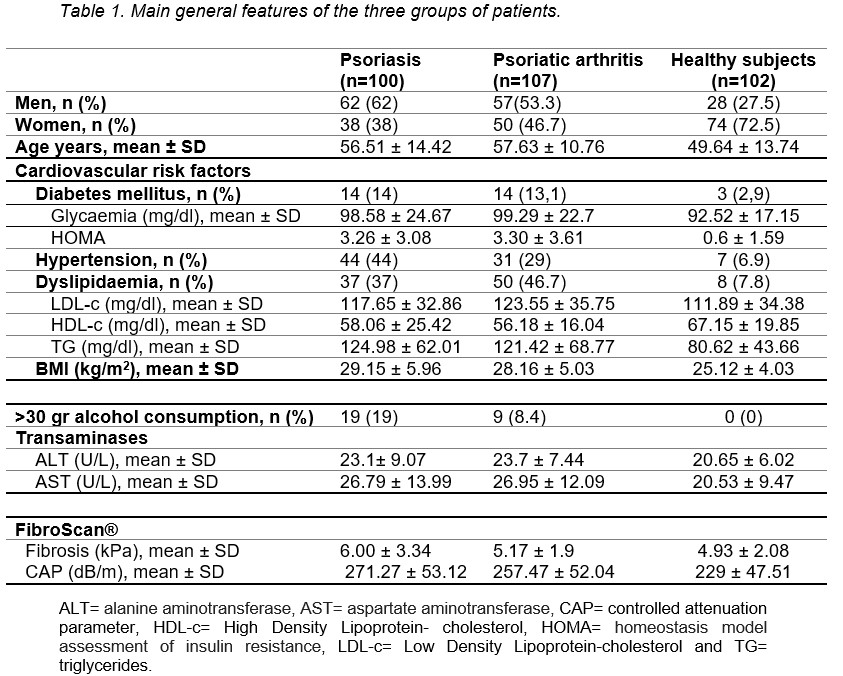
Results: A total of 309 patients were included: 162 women and 147 men, mean age 54.6 ± 13.4 years. Baseline demographic and clinical characteristics for each group are shown in Table 1.
The prevalence of significant fibrosis (≥F2) was 18.3% in the PsD patients and 8.9% in healthy subjects (p=0.031). The prevalence of significant steatosis (≥S1) was 66.3% and 37.6% respectively (p< 0.001). When comparing the PsO and PsA groups, both steatosis and fibrosis were more prevalent in the PsO group (72.4% and 23.5%, respectively) compared to the PsA group (60.6% and 13.5%, respectively), which did not reach statistical differences (p=0.074 and p=0.066 respectively).
Patients with PsO and PsA had a higher BMI, and higher levels of HOMA, triglycerides, ALT and lower levels of HDL cholesterol compared to healthy subjects. LDL cholesterol was higher in the PsA group compared with healthy subjects, but not in the PsO group.
Among the cardiovascular risk factors, only hypertension was statistically significant (p=0.03) in PsO patients with steatosis and fibrosis, although diabetes mellitus, hypertension and obesity were more common in the PsO group than in the PsA group.
Conclusion: The prevalence of liver fibrosis is higher in patients with PsO than in PsA and healthy patients. Steatosis and metabolic risk factors are more prevalent in patients with PsO. This leads to a higher risk of liver fibrosis, so it is advisable to check for steatosis and fibrosis in this group of patients.
To cite this abstract in AMA style:
Plaza-Aulestia N, Ibarguengoitia-Barrena O, Sampedro-Andrada B, San Juan-Lopez C, Morillo-Montañes V, Urionaguena I, Calvo I, Montero Seisdedos D, Vega-Alvarez L, Garcia Llorente J, Vegas Revenga N. Prevalence and Risk Factors of Metabolic Dysfunction-associated Steatotic Liver Disease [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-risk-factors-of-metabolic-dysfunction-associated-steatotic-liver-disease/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-risk-factors-of-metabolic-dysfunction-associated-steatotic-liver-disease/