Session Information
Date: Sunday, October 26, 2025
Title: (0731–0764) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: In clinical practice, 18F-FDG PET-CT often reveals findings suggestive of polymyalgia rheumatica (PMR) in patients with giant cell arteritis (GCA) who lack symptoms or signs indicative of this condition. This study aimed to analyse the prevalence, characteristics, and clinical significance of subclinical PMR in patients with apparently isolated GCA.
Methods: This was a cross-sectional, single-centre study including consecutive patients with newly diagnosed, biopsy-proven GCA and no clinical features of PMR. All underwent 18F-FDG PET-CT at diagnosis. FDG uptake was assessed at anatomical sites typically involved in PMR, including shoulders, sternoclavicular joints, acromioclavicular joints, hips, ischial tuberosities, greater trochanters, symphysis pubis enthesis, and cervical/lumbar interspinous bursae. Visual grading was performed by all raters using liver uptake as reference: 0 (no uptake), 1 (lower than liver), 2 (equal to or greater than liver).
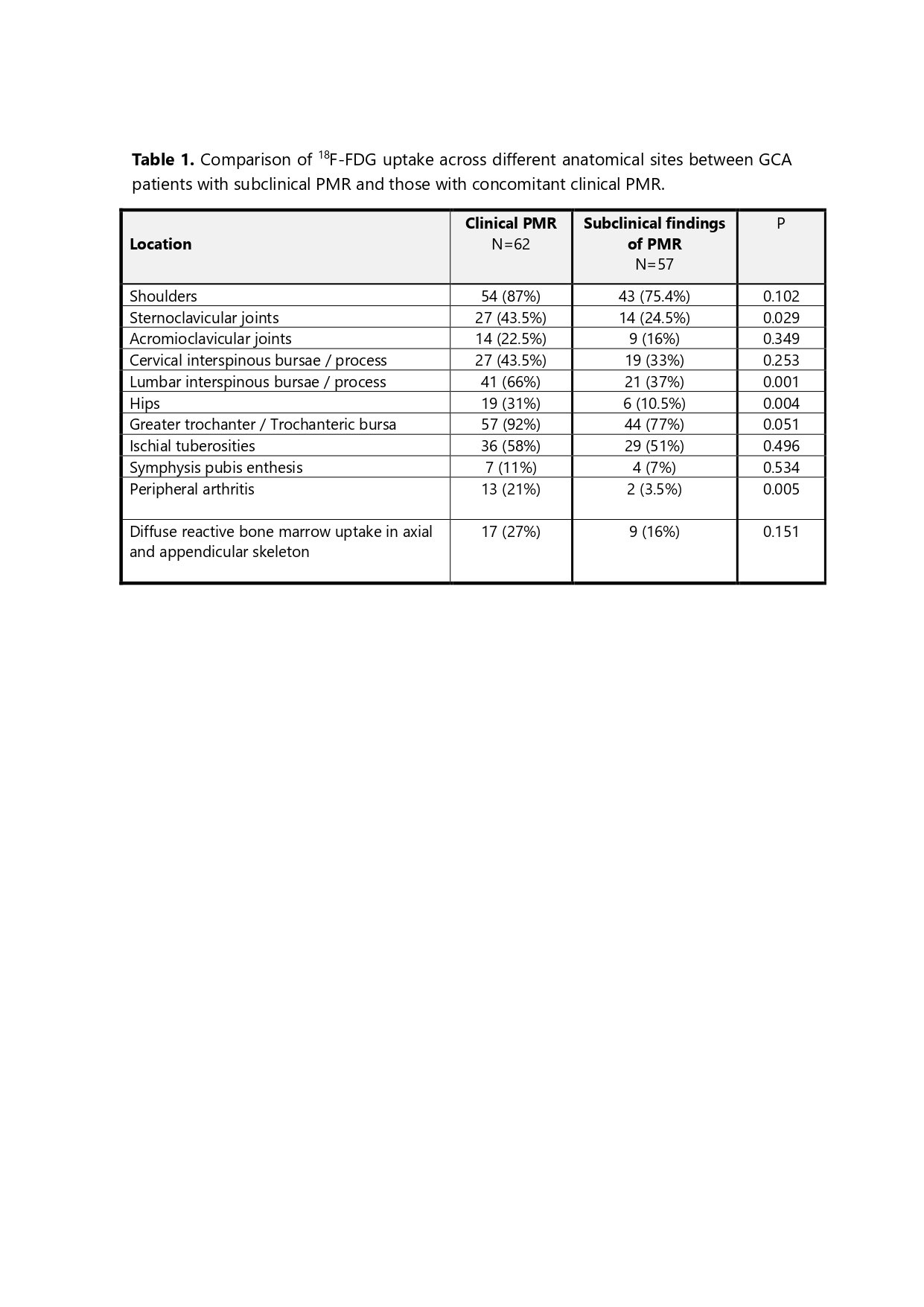
Results: PET findings suggestive of PMR were identified in 57 of 99 patients (57.6%). The distribution of involved anatomical sites is shown in Table 1. The proportion of patients meeting PET-based diagnostic criteria was 26.5% for the Leuven score (≥16), 17% for the Leuven/Groningen score (≥8), 74.0% for the Besançon score, 56.0% for the Yamashita criterion, 54.0% for the Saint-Étienne algorithm, and 42.0% for the Heidelberg algorithm.Compared with patients with GCA without any evidence of PMR (neither clinical nor subclinical), those with subclinical PMR showed a greater frequency of involvement of the thoracic aorta (p=0.080), abdominal aorta (p=0.001), and supra-aortic trunks (p=0.012). No differences were observed at diagnosis regarding cranial manifestations, severe ischaemic complications, intensity of systemic inflammation, or long-term outcomes, including relapse rates, glucocorticoid use and the need for steroid-sparing agents, or mortality.Compared with patients with GCA and clinical PMR (n=62; see table 1), those with subclinical PMR showed lower frequencies of involvement of the sternoclavicular joints (p=0.029), lumbar interspinous bursae (p=0.001), hips (31% vs 10.5%, p=0.004), and peripheral arthritis (p=0.005). The proportion of patients requiring tocilizumab was also significantly lower in this group (29.8% vs 50%; p=0.025).
Conclusion: Subclinical PMR findings are detected by PET-CT in nearly 58% of patients with apparently isolated GCA, supporting the concept of a GCA–PMR spectrum. A substantial proportion fulfilled PMR diagnostic criteria across different PET-based scoring systems. Subclinical PMR was associated with more frequent large-vessel involvement and a distinct anatomical distribution. Its presence does not appear to influence long-term clinical outcomes.
To cite this abstract in AMA style:
Narváez J, Vidal-Montal P, Aguilar-Coll M, Roig Kim M, De Daniel Bisbe L, Cubells M, Fabregat A, Palacios-Olid J, Maymó-Paituvi P, Moragues C, Nolla J. Prevalence and characteristics of subclinical Polymyalgia Rheumatica in patients with Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-characteristics-of-subclinical-polymyalgia-rheumatica-in-patients-with-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-characteristics-of-subclinical-polymyalgia-rheumatica-in-patients-with-giant-cell-arteritis/