Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Risk of thrombosis is elevated in patients with systemic lupus erythematosus (SLE) compared to healthy individuals, especially during the first year after diagnosis. The increased risk for events may be related to co-occurrence of antiphospholipid syndrome (APS) but can also be seen in patients with SLE without APS. Higher SLE disease activity has been hypothesized to contribute to increased risk for thrombotic events. In this study we aim to explore differences in antiphospholipid antibody (aPL) positivity in patients with SLE and venous thromboembolic (VTE) events between Caucasian and AA race. Based on our clinical experience we hypothesize that AA with SLE and VTE events are less likely to have a significant aPL profile compared to Caucasians.
Methods: Patients with diagnosis of SLE and VTE events of Caucasian and AA race were retrieved from the electronic medical record of a large Rheumatology practice based at an academic hospital. All patients had to fulfill ACR and/or SLICC criteria for SLE. Relevant clinical and laboratory characteristics were recorded. Significant aPL profile was defined as presence of moderate-to-high aPL titers (anti-cardiolipin IgG/IgM ≥40 units and/or anti-β2 glycoprotein I IgG/IgM ≥40 units), and/or positive lupus anticoagulant >1.3. Definition of severe SLE included but was not limited to history of lupus nephritis, central nervous system lupus, severe cytopenias, vasculitis, pulmonary hemorrhage, myocarditis, lupus pneumonitis, severe myositis and lupus enteritis. T-test, Wilcoxon rank-sum test, chi-square and Fisher’s exact test were used to compare patient characteristics. Logistic regression was used to explore predictors of a significant aPL profile.
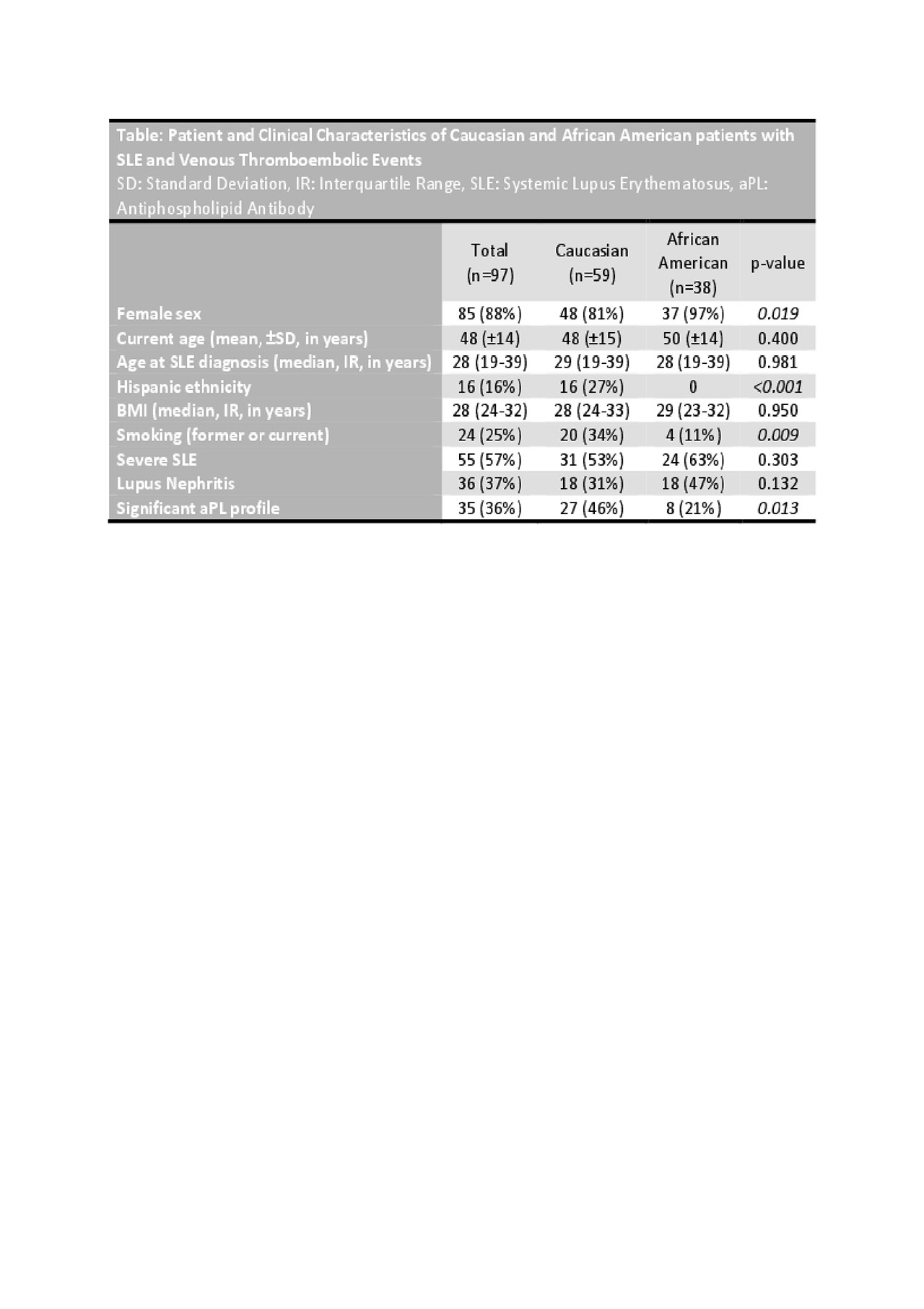
Results: Ninety-seven patients were identified that fulfilled ACR and/or SLICC criteria for SLE, had history of VTE and available aPL tests (Table). Of those, 59 were Caucasian and 38 AA. Twenty-seven (46%) out of 59 Caucasians had a significant aPL profile compared to 8 out of 38 (21%) AA (p=0.013). Recorded VTE events included deep venous thrombosis of extremities, pulmonary embolism, thrombosis of renal, portal, retinal, splenic, mesenteric and sinus vein, and microthrombotic events. Using logistic regression, AA with SLE and VTE events were 66% less likely (95% CI 0.12-0.96, p=0.041) to have a significant aPL profile compared to Caucasians after controlling for age, gender, Hispanic ethnicity, smoking status and SLE severity.
Conclusion: From this study of 97 patients of AA and Caucasian race with history of SLE and VTE events, AA were less likely to have a significant aPL profile compared to Caucasians. These results suggest that a negative aPL profile in AA patients with SLE does not confer a decreased risk for thrombotic events. Further analysis will explore differences in disease activity at time of VTE events between AA and Caucasians.
To cite this abstract in AMA style:
Gkrouzman E, Davis-Porada J, Peng M, Kirou K. Presence of Antiphospholipid Antibodies in Patients with SLE and Venous Thromboembolic Events of African American and Caucasian Race [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/presence-of-antiphospholipid-antibodies-in-patients-with-sle-and-venous-thromboembolic-events-of-african-american-and-caucasian-race/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/presence-of-antiphospholipid-antibodies-in-patients-with-sle-and-venous-thromboembolic-events-of-african-american-and-caucasian-race/