Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The adverse effects of systemic lupus erythematosus (SLE) on maternal and fetal outcomes in pregnancy have been explored mainly in clinic-based cohorts. However, data comparing maternal and fetal outcomes before and after diagnosis of SLE at the population-based level are scarce. The purpose of our study was to assess fetal and maternal outcomes before and after SLE diagnosis.
Methods: We conducted a population-based, retrospective cohort study from a perinatal registry that included all pregnancies in the province between the 1st of January 2002 and 31st of December 2012. SLE was defined as greater than or equal to 2 ICD-9/ICD-10 codes at least 2 months apart and within a 2-year window. SLE exposure was based on diagnosis before or after date of conception. The groups were defined as post-SLE (pregnancy following SLE diagnosis) or pre-SLE (pregnancy preceding SLE diagnosis). We used logistic, Cox and Poisson regression models to evaluate the effects of SLE on perinatal outcomes (small for gestational age [SGA], congenital anomalies (CA), preterm delivery, major infection in baby) and maternal outcomes (major infections). Infant infections were defined as occurring in the first year of life, while maternal infections were only in the first six weeks following delivery. All models were adjusted for maternal prescription medications, comorbidities, prior pregnancy outcomes, and body mass index.
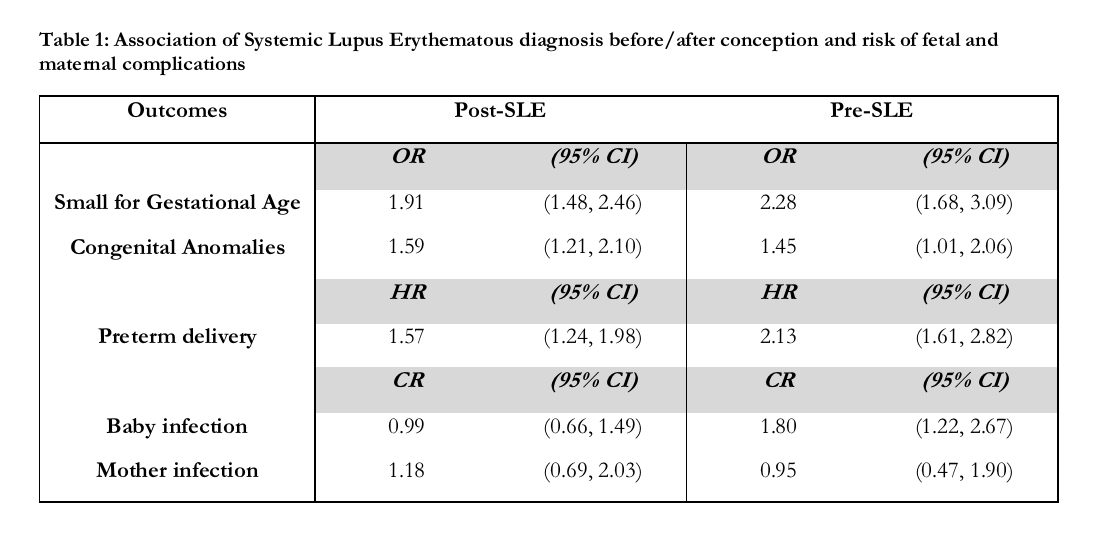
Results: 405,538 total pregnancies were evaluated, with 608 occurring in SLE patients. Among these, 376 pregnancies were post-SLE, and 232 were pre-SLE. In adjusted analyses, the odds ratios (OR) for the association of SLE with having infants born SGA were 1.91 (95% CI 1.48, 2.46) for post-SLE and 2.28 (95% CI 1.68, 3.09) for pre-SLE when compared to non-SLE pregnancies (See Table 1). The adjusted ORs for CA were also increased in both periods (see Table 1). Furthermore, the hazard ratios (HR) for the effect of post- and pre-SLE on preterm delivery were also increased. In adjusted analyses, the count ratios (CR) for the association of SLE with a serious newborn infection were increased only in the pre-SLE group, CR = 1.80 (95% CI 1.22, 2.67), when compared to non-SLE pregnancies. No increased risk for serious maternal infection was seen (see Table 1).
Conclusion: We found an increased risk of SGA, CA, preterm delivery, and serious newborn infection in pregnancies of patients with SLE. The risk was increased even in pregnancies before SLE diagnosis. There was no association between SLE and risk of serious maternal infection.
To cite this abstract in AMA style:
Wade AN, De Vera MA, Sayre EC, Avina-Zubieta JA. Pregnancy Outcomes in Systemic Lupus Erythematous and Pre-Systemic Lupus Erythematous: A Population-Based Cohort Study [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/pregnancy-outcomes-in-systemic-lupus-erythematous-and-pre-systemic-lupus-erythematous-a-population-based-cohort-study/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-outcomes-in-systemic-lupus-erythematous-and-pre-systemic-lupus-erythematous-a-population-based-cohort-study/