Session Information
Date: Tuesday, November 7, 2017
Title: Spondyloarthropathies and Psoriatic Arthritis – Clinical Aspects and Treatment III
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Pregnancy outcomes in patients with ankylosing spondylitis: a nationwide population study.
Background/Purpose: Autoimmune inflammatory diseases influence on pregnancy outcomes. But rare studies have focus on the ankylosing spondylitis (AS) and pregnancy outcomes.
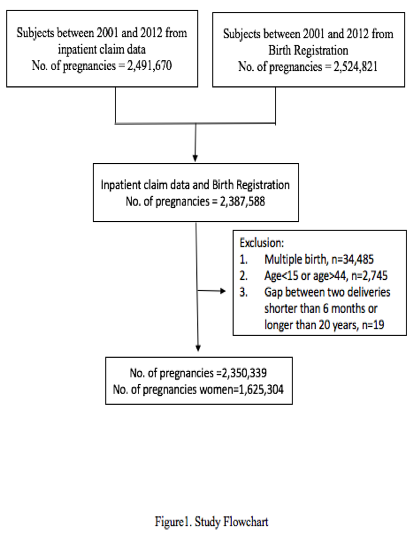
Methods: The primary data source was the National Health Insurance database and national birth registry of Taiwan. We obtained records of all pregnancies in Taiwan between 2001 and 2012 from a national insurance database. Maternal and fetal outcomes were obtained from national birth registry.
Results: We analyzed data from 2,350,339 women between 2001 and 2012 categorized into 2 groups. Subjects in the reference group (2,347,847 women) had no AS diagnosis, and those in the AS group (2,492 women) had diagnosed with AS before pregnancy. Maternal outcomes in patients with AS revealed a higher adjusted odds ratio for Puerperal cerebrovascular disorders (OR 4.05 95% CI 2.02 to 8.12), Preterm labor (OR 1.18 95% CI 1.00 to 1.38), cesarean delivery (OR 1.08 95% CI 1.01 to 1.15), pulmonary edema (OR 4.99 95% CI 1.24 to 20.10) and gestational diabetes (OR 1.16 95% CI 1.02 to 1.34). The neonatal outcomes in AS group showed a higher adjusted OR for poorer 1 minute Apgar score (<7) (OR 1.38 95% CI 1.10 to 1.75), poorer 5 minute Apgar score (<7) (OR 1.60 95% CI 1.02 to 2.52), fetal abnormalities (OR 1.20 95% CI 1.03 to 1.39), chromosomal abnormalities (OR 1.72 95% CI 1.15 to 2.59) and unspecific abnormalities (OR 1.28 95% CI 1.01 to 1.62).
Conclusion: Patients with AS were associated with higher prevalence of adverse birth outcomes.
Table 1. Comparison of maternal outcomes between pregnancies associated with maternal AS or not.
|
Pregnancies N (%) |
Crude Odds ratio (95% CI) |
Adjusted Odds ratio_ (95%CI) |
|||||||
|
Without AS (n= 2,347,847)
|
With AS (n=2,492) |
||||||||
|
Overall outcomes
|
|
|
|
|
|
|
|
|
|
|
Death _30 days post-partum |
314 |
(0.01)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Death _1 year post-partum
|
793
|
(0.03)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Cardiovascular |
|
|
|
|
|
|
|
|
|
|
Acute myocardial |
111 |
(0.00)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Aneurysm |
52 |
(0.00)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Cardiac arrest/ ventricular fibrillation |
116 |
(0.00)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Heart failure |
144 |
(0.01)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Shock |
1,191 |
(0.05)
|
2
|
(0.08)
|
1.58
|
(0.40-6.28)
|
1.28
|
(0.32-5.14)
|
|
|
Conversion of cardiac rhythm |
555 |
(0.02)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Pregnancy-related hypertension |
53,984 |
(2.30)
|
65
|
(2.61)
|
1.14
|
(0.89-1.48)
|
0.91
|
(0.72-1.16)
|
|
|
Gestational hypertension |
23,028 |
(0.98)
|
25
|
(1.00)
|
1.03
|
(0.69-1.54)
|
0.78
|
(0.52-1.15)
|
|
|
Puerperal cerebrovascular disorders |
1,705 |
(0.07)
|
8
|
(0.32)
|
4.33
|
(2.12-8.85)*
|
4.05
|
(2.02-8.12)*
|
|
|
Thrombotic embolism |
214 |
(0.01)
|
2
|
(0.08)
|
4.59
|
(0.65-32.3)
|
3.8
|
(0.53-27.1)
|
|
|
Complication during delivery |
|
|
|
|
|
|
|
|
|
|
Amniotic fluid embolism |
232 |
(0.01)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Antepartum hemorrhage |
209,662 |
(8.93)
|
257
|
(10.31)
|
1.18
|
(1.03-1.34)*
|
1.10
|
(0.97-1.24)
|
|
|
Postpartum hemorrhage due to atony |
12,621 |
(0.54)
|
19
|
(0.76)
|
1.43
|
(0.91-2.24)
|
1.17
|
(0.75-1.84)
|
|
|
Postpartum hemorrhage not due to atony |
3,501
|
(0.15)
|
4
|
(0.16)
|
1.08
|
(0.41-2.88)
|
0.89
|
(0.33-2.37)
|
|
|
Severe postpartum hemorrhage |
63,287 |
(2.70)
|
83
|
(3.33)
|
1.24
|
(0.99-1.56)
|
1.23
|
(0.99-1.53)
|
|
|
Preterm labor |
106,014 |
(4.52)
|
148
|
(5.94)
|
1.34
|
(1.13-1.59)*
|
1.18
|
(1.00-1.38)*
|
|
|
Premature rupture of membranes |
83 |
(0.00)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Chorioamnionitis |
8,057
|
(0.34)
|
7
|
(0.28)
|
0.80
|
(0.38-1.67)
|
0.75
|
(0.36-1.57)
|
|
|
Cesarean delivery |
781,237 |
(33.27)
|
992
|
(39.81)
|
1.33
|
(1.23-1.44)*
|
1.08
|
(1.01-1.15)*
|
|
|
Induction of labor |
117 |
(0.00)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Surgical complications |
|
|
|
|
|
|
|
|
|
|
Severe anesthesis complications
|
302 |
(0.01)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Thorax, abdomen, and pelvis injuries |
968 |
(0.04)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Intracranial injuries |
5,585 |
(0.24)
|
4
|
(0.16)
|
0.65
|
(0.24-1.80)
|
0.79
|
(0.30-2.10)
|
|
|
Blood transfusion |
13,296 |
(0.57)
|
15
|
(0.60)
|
1.09
|
(0.66-1.80)
|
0.91
|
(0.55-1.52)
|
|
|
Hysterectomy |
1,859 |
(0.08)
|
3
|
(0.12)
|
1.51
|
(0.49-4.66)
|
1.26
|
(0.41-3.91)
|
|
|
Operations on heart and pericardium |
1,605 |
(0.07)
|
2
|
(0.08)
|
1.22
|
(0.31-4.82)
|
0.88
|
(0.22-3.51)
|
|
|
Other |
|
|
|
|
|
|
|
|
|
|
Adult respiratory distress syndrome |
1,011 |
(0.04)
|
2
|
(0.08)
|
1.80
|
(0.45-7.16)
|
1.46
|
(0.36-5.84)
|
|
|
Sepsis |
5,867 |
(0.25)
|
8
|
(0.32)
|
1.29
|
(0.65-2.58)
|
1.06
|
(0.53-2.12)
|
|
|
Disseminated intravascular coagulation |
1,541 |
(0.07)
|
2
|
(0.08)
|
1.22
|
(0.31-4.82)
|
0.94
|
(0.24-3.77)
|
|
|
Preeclampsia |
37,046 |
(1.58)
|
49
|
(1.97)
|
1.25
|
(0.93-1.68)
|
1.03
|
(0.78-1.36)
|
|
|
pulmonary edema |
330 |
(0.01)
|
2
|
(0.08)
|
5.86
|
(1.47-23.4)*
|
4.99
|
(1.24-20.10)*
|
|
|
Temporary tracheostomy |
103 |
(0.00)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Ventilation |
19,810 |
(0.84)
|
31
|
(1.24)
|
1.50
|
(1.06-2.14)*
|
1.04
|
(0.73-1.49)
|
|
|
Seizures among preeclamptic patients
|
1,690 |
(0.07)
|
0
|
(0.00)
|
N/A
|
N/A
|
|||
|
Gestational diabetes |
126,485 |
(5.39)
|
204
|
(8.19)
|
1.58
|
(1.36-1.83)*
|
1.16
|
(1.02-1.34)*
|
|
_Adjusted for age, infant sex, Charlson comorbidity index, urbanization, income, occupation, birth year, maternal nationality
*p<0.05
Table 2. Comparison of neonatal outcomes between pregnancies associated with maternal AS or not.
|
Pregnancies N (%) |
|
|
||||||
|
Without AS (n= 2,347,847)
|
With AS (n=2,492) |
Crude Odds ratio (95% CI) |
Adjusted Odds ratio (95% CI)_ |
|||||
|
Stillbirth |
17,346 |
(0.74)
|
17
|
(0.68)
|
0.93
|
(0.57-1.49)
|
0.81
|
(0.50-1.30)
|
|
explained stillbirth |
1,766
|
(0.08)
|
3
|
(0.12)
|
1.60
|
(0.52-4.97)
|
1.38
|
(0.44-4.28)
|
|
unexplained stillbirth |
15,580
|
(0.66)
|
14
|
(0.56)
|
0.85
|
(0.50-1.44)
|
0.75
|
(0.44-1.26)
|
|
Low birth weight (<2500 g) |
151,048 |
(6.43)
|
173
|
(6.94)
|
1.19
|
(1.03-1.38)*
|
1.06
|
(0.91-1.22)
|
|
Prematurity (<37 week) |
178,059
|
(7.58)
|
219
|
(8.79)
|
1.10
|
(0.94-1.30)
|
1.10
|
(0.96-1.26)
|
|
Small for gestational age |
227,984 |
(9.71)
|
221
|
(8.87)
|
0.91
|
(0.78-1.05)
|
0.97
|
(0.85-1.11)
|
|
Large for gestational age |
231,066
|
(9.84)
|
227
|
(9.11)
|
0.91
|
(0.79-1.05)
|
0.85
|
(0.74-0.97)
|
|
APGAR SCORE 1 min (<7) |
46,844 |
(2.00)
|
71
|
(2.85)
|
1.45
|
(1.14-1.83)*
|
1.38
|
(1.10-1.75)*
|
|
APGAR SCORE 5 min (<7) |
12,194
|
(0.52)
|
19
|
(0.76)
|
1.48
|
(0.94-2.32)
|
1.60
|
(1.02-2.52)*
|
|
Fetal distress |
116,442 |
(4.96)
|
125
|
(5.02)
|
1.00
|
(0.83-1.20)
|
1.00
|
(0.84-1.19)
|
|
Fetal abnormalities, any |
105,705
|
(4.50)
|
165
|
(6.62)
|
1.52
|
(1.29-1.79)*
|
1.20
|
(1.03-1.39)*
|
|
Central nervous system malformations |
10,085 |
(0.43)
|
8
|
(0.32)
|
0.73
|
(0.36-1.48)
|
0.67
|
(0.33-1.34)
|
|
Chromosomal abnormalities |
10,207
|
(0.43)
|
23
|
(0.92)
|
2.15
|
(1.40-3.30)*
|
1.72
|
(1.15-2.59)*
|
|
Hereditary disease in family possible affecting fetus |
1,863
|
(0.08)
|
4
|
(0.16)
|
1.95
|
(0.66-5.71)
|
1.55
|
(0.58-4.12)
|
|
Suspected damage due to viral or other disease in the mother |
3,122
|
(0.13)
|
7
|
(0.28)
|
2.26
|
(1.09-4.69)*
|
1.62
|
(0.77-3.40)
|
|
Suspected damage due to drugs or radiation |
923
|
(0.04)
|
0
|
(0.00)
|
N/A
|
N/A
|
||
|
decreased fetal movements |
33,970
|
(1.45)
|
59
|
(2.37)
|
1.66
|
(1.28-2.17)*
|
1.17
|
(0.91-1.51)
|
|
Other/unspecified abnormalities |
42,411
|
(1.81)
|
69
|
(2.77)
|
1.59
|
(1.24-2.04)*
|
1.28
|
(1.01-1.62)*
|
_Adjusted for age, infant sex, Charlson comorbidity index, urbanization, income, occupation, birth year, maternal nationality
*p<0.05
To cite this abstract in AMA style:
Fang YF. Pregnancy Outcomes in Patients with Ankylosing Spondylitis: A Nationwide Population Study [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/pregnancy-outcomes-in-patients-with-ankylosing-spondylitis-a-nationwide-population-study/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-outcomes-in-patients-with-ankylosing-spondylitis-a-nationwide-population-study/