Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Although the overall systemic lupus (SLE) patient population is racially and ethnically diverse, many study populations are homogeneous. We assembled a diverse group of patients from Kaiser Permanente Northern California (KPNC), leveraging their integrated health care delivery system that includes primary and specialty care, as well as its own pharmacy. Our goal was to describe this diverse, contemporary cohort and their pregnancy outcomes.
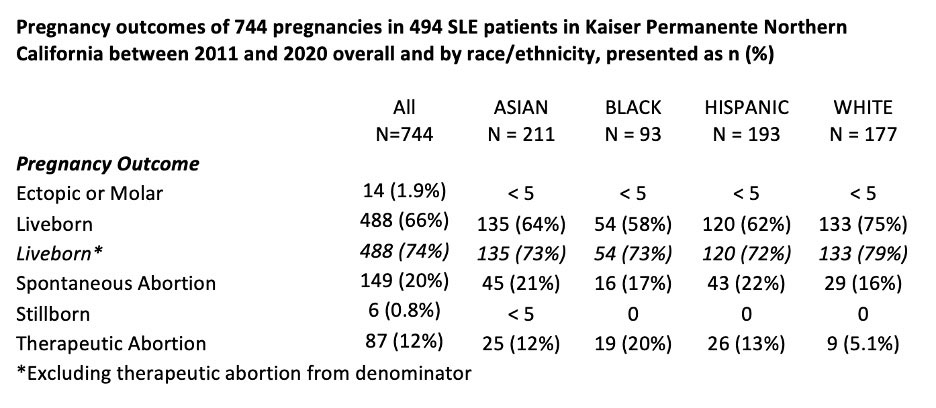
Methods: We used KPNC electronic data including the Obstetric Database (POD) of all pregnancies from 2011-2020 regardless of outcome. SLE was defined as ≥2 ICD coded visits ≥7 days apart and individuals included if a pregnancy was observed in POD (2011- 2020). We required qualifying SLE-coded encounters occurred by the last menstrual period (LMP). We summarized patient descriptives, medication orders, and healthcare utilization, and provided frequencies of medication fills and pregnancy outcomes (livebirth, stillbirth, spontaneous abortion, therapeutic abortion, ectopic, molar) overall, and stratified by race/ethnicity. We also calculated a secondary livebirth rate excluding therapeutic abortions.
Results: We identified 744 pregnancies among 494 patients with SLE in KPNC from 2011-2020: 28% were Asian, 26% were Hispanic, 24% were White, 12% were Black, 5.8% were Multiracial, 1.1% were Islander, 0.9% were Native American, and the remaining 1.6% (n=12) had unknown race/ethnicity. We observed a 66% livebirth “rate” overall, 20% pregnancies ending by spontaneous abortion and 12% therapeutic abortions. We noted some variability by race/ethnicity for the 4 largest groups. When excluding therapeutic abortions, we noted comparable livebirth “rates” across rate/ethnic groups (see Table).
Most received rheumatologic care (94.6%) and 21.9% had ≥1 nephrology visit from SLE presentation through pregnancy. During this same period, 82% were prescribed an antimalarial, 69.2% had ≥1 prescription for corticosteroids, and 92.9% were prescribed NSAIDs. From 3 months pre-LMP through the first trimester, 94.5% received care from OB/GYN, 83.7% had a visit with primary care/family medicine, and 52.8% had at least one visit with a rheumatologist. Main prescriptions filled during pregnancy were 46% hydroxychloroquine (HCQ), 22% corticosteroids, and 15% NSAIDs/anti-inflammatories.
Conclusion: In this diverse cohort, we found that nearly all patients with lupus received medical care in early pregnancies, and >50% saw a rheumatologist. Medication use during pregnancy was relatively low, with only 46% filling at least 1 prescription for HCQ. The live birth “rate” in SLE pregnancy is often reported as 80-85% in a range of cohorts and clinical populations. We found that the overall live birth rate was 66% with some disparities by race, which increased to around 74% when we excluded therapeutic abortions from the denominator.
To cite this abstract in AMA style:
Simard J, Liu E, Chakravarty E, Rector A, Cantu M, Kuo D, Shaw G, Druzin M, Weisman M, Hedderson M. Pregnancy Outcomes in a Diverse Lupus Cohort [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/pregnancy-outcomes-in-a-diverse-lupus-cohort/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-outcomes-in-a-diverse-lupus-cohort/