Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Giant Cell Arteritis (GCA) is the most common systemic vasculitis in North America, typically affecting Caucasian female adults over 50 years of age. Flares and relapses requiring increased and prolonged steroidal medication remains a common trend in patients with GCA. The adverse effects of steroid therapy, and the morbidity and mortality associated with relapsing GCA, is well described however, predictors of relapse remains an understudied area.
Methods: A retrospective chart analysis was performed on 400 patients with an associated ICD10 code diagnosis of GCA seen at Loma Linda University Health from 2013 to 2020. 60 patients were identified with confirmed diagnosis of GCA based on either a positive temporal artery biopsy or meeting the ACR 1990 GCA classification criteria confirmed by a Rheumatologist. We used Pearson’s chi-square to test for independence between demographic, clinical categorical variables, and relapse status. We then used logistic regression to model the relapse binary outcome regressed on permanent vision loss, new onset headache, fever, anterior ischemic optic neuritis, abnormal vascular ultrasound, and pulse steroid as predictor variables. We set alpha equal to 0.05 for statistical significance.
Results: A total of 60 patients were included, of which 46 were female, with an average age of 71 years old and BMI of 28. In our cohort, relapse was defined as an increase in prednisone dose by ≥10 mg for at least two weeks within the first 12 months of GCA diagnosis.
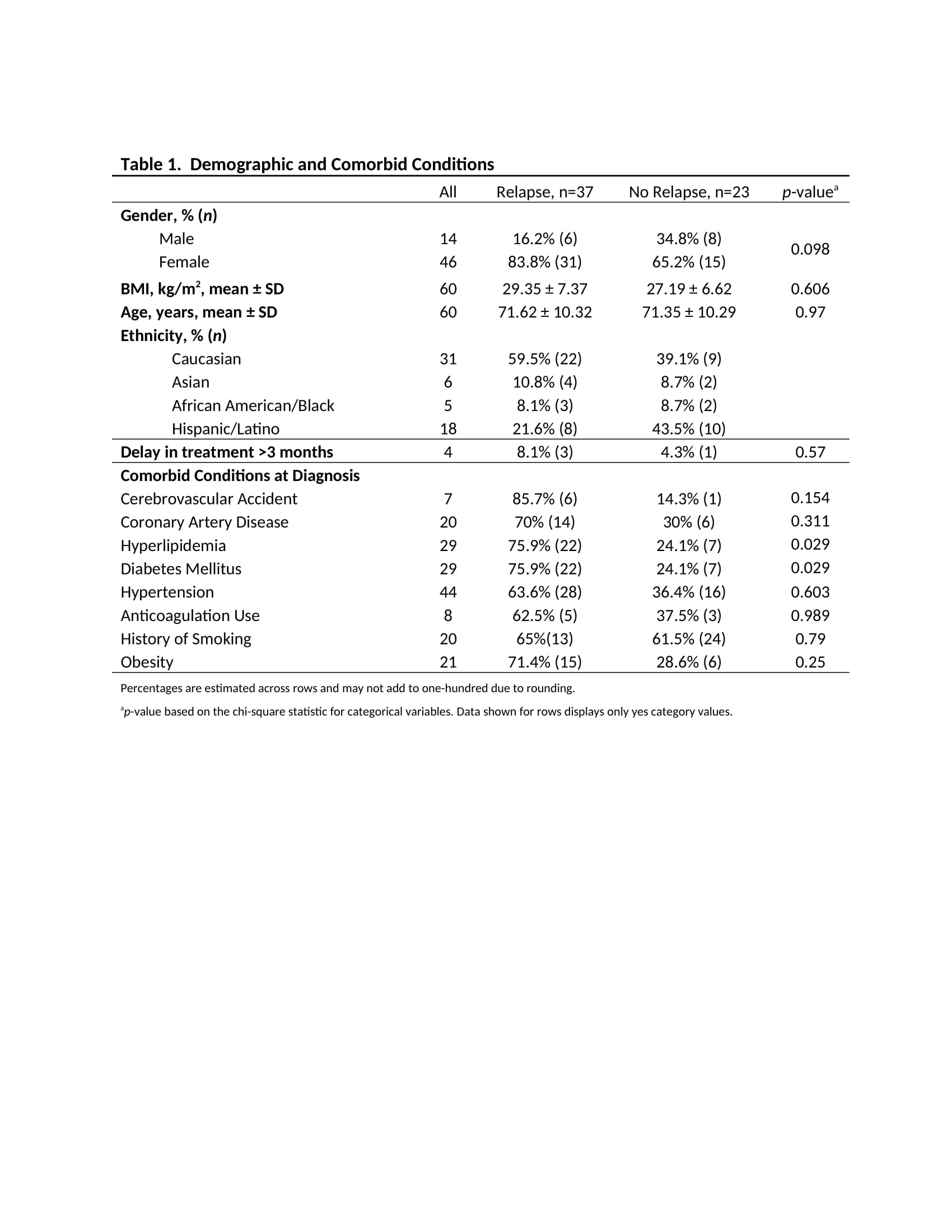
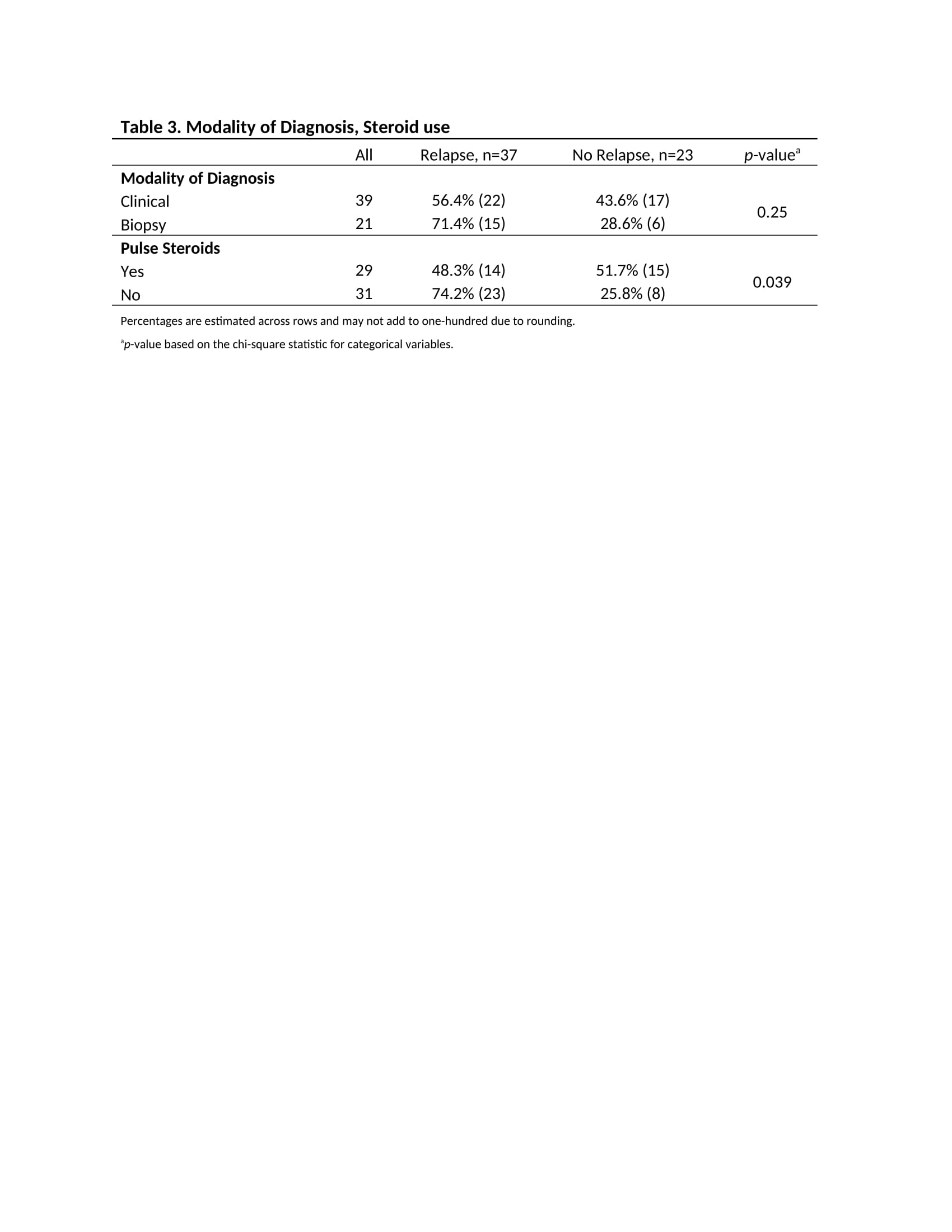
Overall, Caucasians had a higher rate of relapse when compared to other ethnicities, other demographic information was similar between the two groups (Table 1). We found that Hyperlipidemia (HLD), Diabetes Mellitus (DM), and the use of pulse steroids were not independent of relapse status. Those with HLD were more likely to relapse compared to those without HLD (p=0.029). The same outcomes were seen in DM (Table 1). We noted that a higher proportion of patients who relapsed were also those who did not receive pulse steroids (p=0.039) (Table 3). Furthermore, the use of pulse steroids at the time of diagnosis decreased the odds of relapse in this group of patients [OR 0.325 (95% CI 0.110, 0.961)].
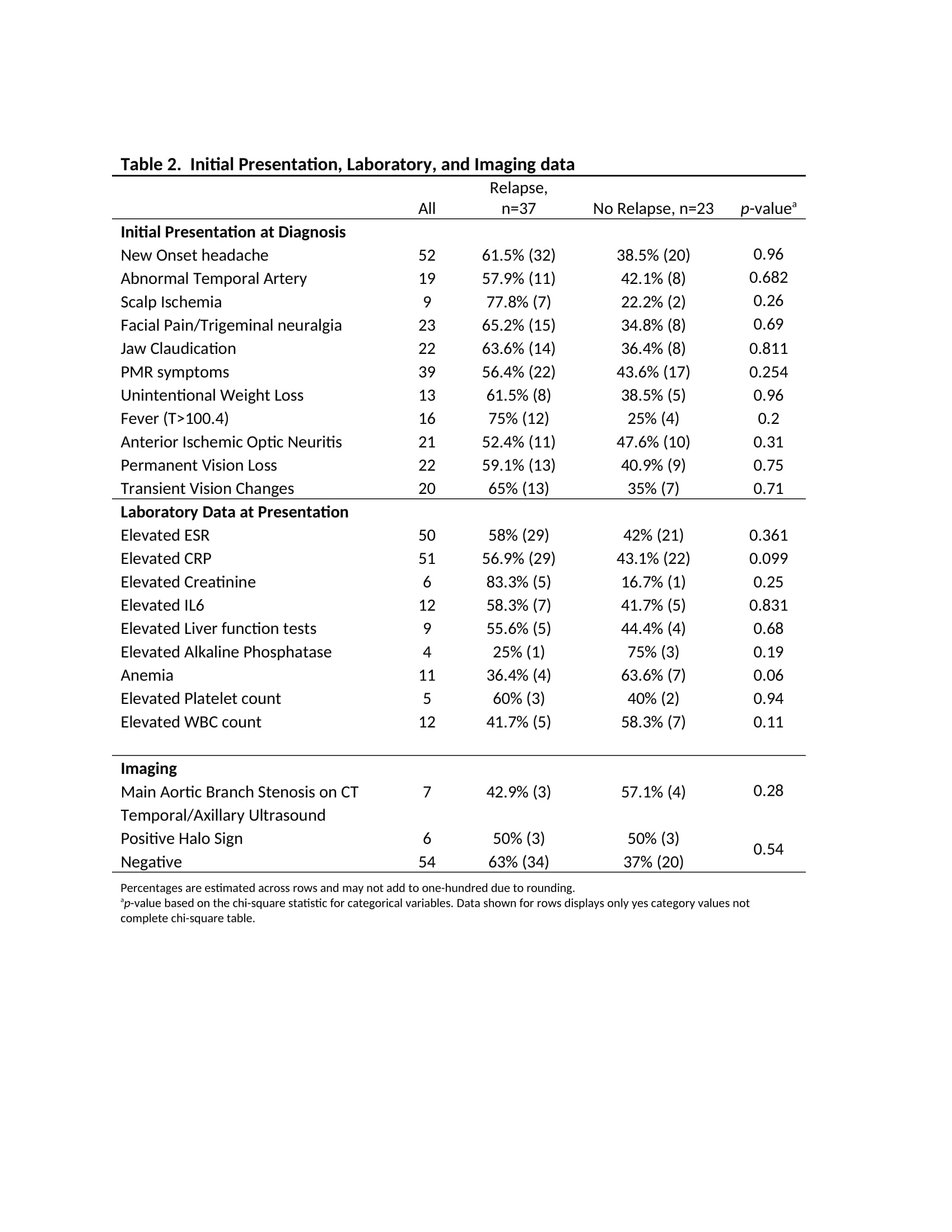
Those in the relapse group also had a higher proportion of Cerebrovascular Accidents, Coronary Artery Disease, Hypertension, Obesity, elevated creatinine, and were on anticoagulation treatment at the time of diagnosis. A higher proportion of the relapse group presented with new onset headache, jaw claudication, scalp ischemia, facial pain/trigeminal neuralgia, and fever (Table 1). In addition, this group were more likely to have been diagnosed via positive temporal artery biopsy (Table 3).
Conclusion: In our cohort, we found patients with comorbidities such as HLD and DM, as well as patients who did not receive pulse steroids were more likely to relapse within the first 12 months of GCA diagnosis. A few clinical manifestations at the time of diagnosis were associated with higher rates of relapse. Our findings suggest certain clinical manifestations and patient comorbidities may provide meaningful insight in relapse prediction. Larger scale studies are required to replicate our findings.
To cite this abstract in AMA style:
D'Anna K, Lim D, Salto L, Hojjati M. Predictors of Relapse in Giant-Cell Arteritis: A Retrospective Single Center Analysis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/predictors-of-relapse-in-giant-cell-arteritis-a-retrospective-single-center-analysis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-relapse-in-giant-cell-arteritis-a-retrospective-single-center-analysis/