Session Information
Session Type: ARP Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Our aim was to determine whether demographics, clinical characteristics or appendicular joint osteoarthritis predict the incidence and worsening of lumbar spine disc space narrowing (DSN), facet joint OA (FOA), osteophytes (OST), and spondylolisthesis.
Methods: These analyses used baseline (2006-2010) and follow-up (2013-2015) data from the Johnston County OA Project. Paired (baseline and follow-up) lumbar spine radiographs were graded for OST and DSN (0-3), spondylolisthesis (0-5) and FOA (present or absent). Incidence was defined as the absence of a specific radiographic feature at baseline and the presence of that feature at follow-up. Worsening was defined as ≥ 1-unit increase from baseline to follow-up for a given radiographic feature. Demographic characteristics of age, race (African American vs. white), and sex, clinical characteristics of the history of low back symptoms, comorbidities (diabetes, high blood pressure and ever smoking), and back injury were determined by self-report. Body mass index (BMI) variables of weight and height were measured at the research clinic visit with obesity defined as BMI≥30 kg/m2. Appendicular OA was defined as a Kellgren-Lawrence grade >2 at the knee or hip or a grade ≥2 in a minimum of one distal interphalangeal (IP) joint and 2 other joints (IP or carpometacarpal) at the hand. Weibull models, which account for interval censoring, were used to estimate adjusted (simultaneously for all predictors) hazards ratios (aHR) and 95% confidence intervals (CI) and whether the effects differed in those with and without low back symptoms.
Results: Paired lumbar spine radiograph scores were available for 819 participants. Baseline characteristics were mean age 66.1 (SD 7.5), mean BMI 31.5 (6.1) kg/m2; 67.9% were women, 31.8% were African American, and 39.6% had radiographic knee OA, 35.5% hip OA, 32.0% hand OA, and 34.8% had low back symptoms. The incidence of OST, FOA, DSN and spondylolisthesis was 59.0%, 11.1%, 38.1% and 9.1%, respectively. Worsening of OST, DSN, and spondylolisthesis occurred in 33.8%, 23.9% and 7.8%, respectively.
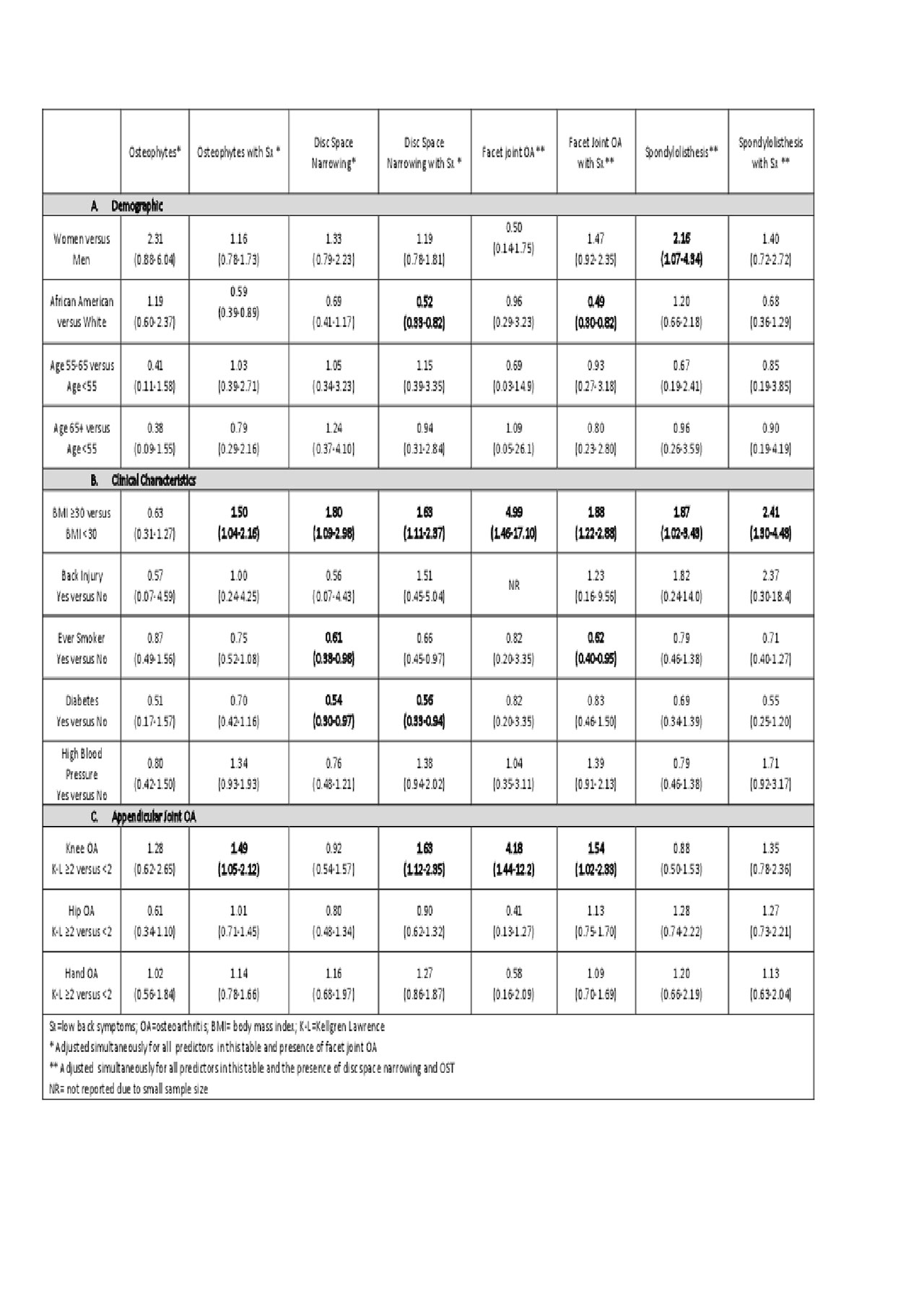
AAs were less likely to develop FOA with symptoms and DSN with symptoms. Women were more likely to develop spondylolisthesis. (Table 1a) Obesity was a predictor of incidence for all lumbar spine features. Smokers were less likely to develop DSN and FOA with symptoms. Participants with diabetes were less likely to develop DSN with symptoms and without. (Table 1b) Presence of Knee OA predicted incident: vertebral OST with symptoms, DSN with symptoms, FOA and FOA with symptoms. (Table 1c)
Women were more likely to develop worsening of DSN. AAs were less likely to develop worsening of OST and DSN with symptoms. (Table 2a) Obesity was a predictor of worsening for all lumbar spine features. Diabetes was a predictor of osteophyte worsening. (Table 2b) Appendicular joint OA did not predict worsening of spine OA features. (Table 2c)
Conclusion: Obesity consistently predicted incidence and worsening of lumbar spine radiographic features with and without low back symptoms. Notable variation in other predictors for incidence and worsening suggest that the etiological process of degeneration may differ for some radiographic features.
To cite this abstract in AMA style:
Goode A, Cleveland R, Hu D, George S, Byers Kraus V, Schwartz T, Gracely R, DeFrate L, Jordan J, Golightly Y. Predictors of Incident and Worsening Lumbar Spine Degeneration: The Johnston County Osteoarthritis Project [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/predictors-of-incident-and-worsening-lumbar-spine-degeneration-the-johnston-county-osteoarthritis-project/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-incident-and-worsening-lumbar-spine-degeneration-the-johnston-county-osteoarthritis-project/