Session Information
Session Type: Abstract Submissions
Session Time: 5:30PM-7:00PM
Background/Purpose: Factors affecting treatment (Rx) responses in juvenile dermatomyositis (JDM) are not well understood. We examined a large JDM registry for predictors of excellent Rx responses, including final discontinuation of corticosteroid therapy (CS-DC), complete clinical response (CCR, clinically inactive disease for ≥6 continuous mths on Rx), and remission (inactive disease for ≥6 continuous mths off all Rx).
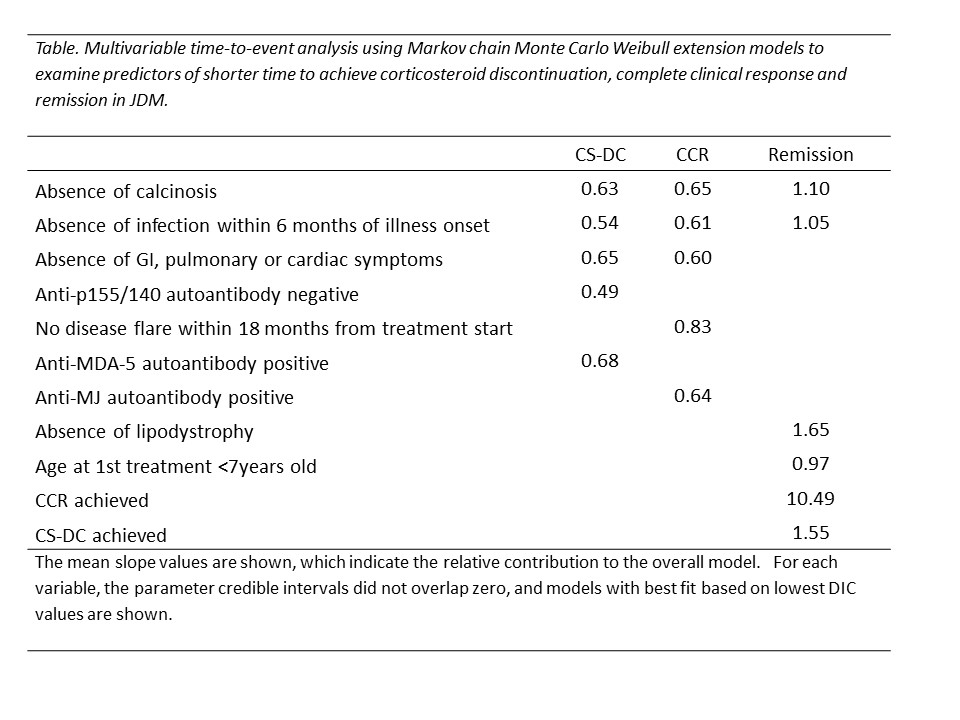
Methods: A retrospective review of Rx responses in 305 pts with probable or definite JDM was conducted. The median Rx duration was 30 mths [IQR 19-57 mths] and follow-up duration was 43 mths [IQR 22-74 mths]. We evaluated the probability of achieving CS-DC, CCR, and remission by Weibull time-to-event models. Significant univariable predictors of each outcome (Log rank P<0.05) were examined in multivariable time-to-event analysis using Markov chain Monte Carlo Weibull extension models. The conditional probability of each outcome was also evaluated using Bayesian network models.
Results: Fifty-two percent (159 pts) experienced final CS-DC and the probability of achieving CS-DC was 9.7% at 1 year, 35% at 3 years and 57% at 5 years after initial Rx. Thirty-three percent (99 pts) achieved CCR and the probability of achieving CCR was 7.9% at 1 year, 27% at 3 years and 44% at 5 years after Rx start. Twenty-six percent (80 pts) achieved remission, including 31 pts who achieved remission without CCR first. The probability of remission was 3.2% at 1 year, 16% at 3 years, and 31% at 5 years after Rx start. The probability of CCR or remission was found to be conditional: For CCR, the probability of attaining CCR given CS-DC was 47%; when CS-DC was not attained, the probability of achieving CCR was 19%. For remission, when CS-DC and CCR were achieved the probability of achieving remission was 66%. When CS-DC and CCR were not achieved, the probability of achieving remission was 3.5%. If either CS-DC or CCR were achieved in isolation, the probability of achieving remission was 27%.
The absence of calcinosis and infection within 6 months of illness onset were associated with shorter times to achieve these 3 outcomes in multivariable modeling (Table). The absence of GI, pulmonary or cardiac symptoms was associated with shorter times to achieve CS-DC and CCR. MDA5 Abs and lack of p155/140 Abs, but MJ Abs and lack of early flare were associated with shorter times to CS-DC and CCR, respectively. Achievement of CCR strongly predicted shorter time to remission, with CS-DC, absence of lipodystrophy and younger age at first Rx as other predictors.
Conclusion: A large proportion of JDM patients achieve positive Rx responses, including CS-DC, CCR, and remission, although timelines for these important outcomes are relatively long. Factors associated with shorter times to achieve these Rx outcomes include selected clinical features, MSAs, and environmental factors.
To cite this abstract in AMA style:
Kishi T, Warren-Hicks W, Ward M, Bayat N, Wu L, Mamyrova G, N. Targoff I, Miller F, Rider LG. Predictors of Corticosteroid Discontinuation, Complete Clinical Response and Remission in Patients with Juvenile Dermatomyositis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 4). https://acrabstracts.org/abstract/predictors-of-corticosteroid-discontinuation-complete-clinical-response-and-remission-in-patients-with-juvenile-dermatomyositis/. Accessed .« Back to 2017 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-corticosteroid-discontinuation-complete-clinical-response-and-remission-in-patients-with-juvenile-dermatomyositis/