Session Information
Date: Sunday, October 21, 2018
Title: Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I: Comorbidities
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: We previously reported higher prevalence, burden and more vulnerable occult coronary plaque composition in patients with rheumatoid arthritis (RA) compared to age and gender-matched non-autoimmune disease controls. We now explore the predictors of change in coronary atherosclerosis burden and plaque composition in RA patients with a follow-up non-invasive interrogation of coronary anatomy.
Methods: One hundred participants with a baseline 64-slice coronary computed tomography angiography (CCTA) for atherosclerosis interrogation, underwent a follow-up assessment in a mean of 83±3.6 months. Plaque load was evaluated with 3 quantitative scores: segment involvement score (SIS) reflected the number of segments with plaque; segment stenosis score (SSS) reported the cumulative stenosis grade conferred by plaque over all evaluable segments and the plaque burden score (PBS) described the cumulative plaque size over all evaluable segments. Plaque composition was defined as non-calcified (NCP), mixed (MP) or calcified (CP). Coronary artery calcium score (CAC) was quantified by the Agatston method. Multivariate linear and logistic regression models evaluated independent determinants of change in total, NCP, MP and CP plaque burden; multinomial logistic regression models compared predictors of individual plaque type burden progression or regression against non-progressors.
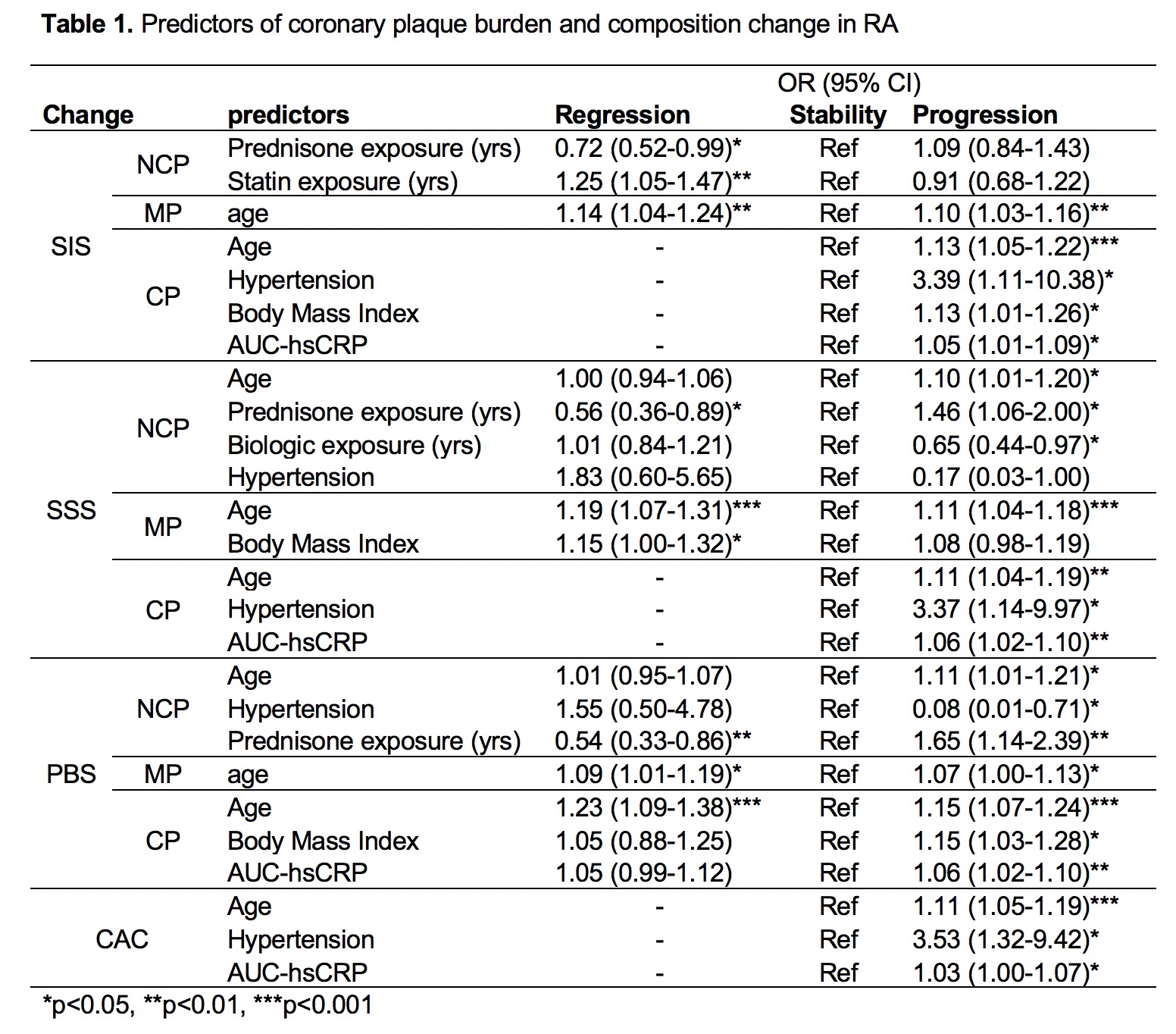
Results: Total plaque burden increased in 41%, remained stable in 41% and decreased in 18%. Duration of prednisone exposure in-between studies, and age independently predicted total plaque burden change (all p<0.05). NCP regression was predicted by lower prednisone and higher statin duration exposure, whereas NCP progression was forecasted by longer prednisone and shorter biologic DMARD inter-scan exposure, older age, and higher prevalence of HTN compared to non-progressors (all p<0.05). CP-progressors were older, with higher cumulative inflammatory burden [area under the curve for c-reactive protein (AUC-hsCRP)], more obese and with greater prevalence of hypertension, and (all p<0.05) than non-progressors. Finally, CAC increase was independently predicted by older age, hypertension and cumulative inflammatory burden (all p<0.05).
Conclusion: Cardiac risk factors, inflammation and duration of exposure to medications such as prednisone, biologics and statins significantly and differentially impacted coronary plaque burden and composition change over time in RA.
To cite this abstract in AMA style:
Karpouzas G, Ormseth S, Hernandez E, Budoff M. Predictors of Change in Coronary Plaque Burden and Composition in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/predictors-of-change-in-coronary-plaque-burden-and-composition-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-change-in-coronary-plaque-burden-and-composition-in-patients-with-rheumatoid-arthritis/