Session Information
Date: Monday, November 9, 2020
Title: Pediatric Rheumatology – Clinical II: Outcomes & Care Delivery (1983–1987)
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: The transition from pediatric to adult care is a vulnerable period and is linked to increased healthcare utilization and poor outcomes. We sought to identify risk factors associated with an unsuccessful transfer to adult care in childhood-onset systemic lupus erythematosus (cSLE).
Methods: A retrospective analysis of patients with cSLE seen in adult public or private rheumatology clinics was performed. Outcomes of interest were development of end-stage renal disease (ESRD) or death and time to first hospitalization following the final pediatric rheumatology visit. Independent variables included sociodemographic and disease characteristics. Pediatric factors influencing ESRD or death were assessed using Chi-square, Fisher’s test, or the Wilcoxon rank-sum test. A stepwise multivariable logistic regression model to predict ESRD or death was used. Pediatric factors influencing time to first hospitalization were assessed using the log-rank test. Stepwise multivariable Cox regression analysis was performed to define predictors of time to adult hospitalization.
Results: Of 190 patients with cSLE, 21 (11%) developed ESRD and 9 (5%) died following the final pediatric rheumatology visit. As seen in Figure 1, ESRD or death were more common among patients of Black race or Hispanic ethnicity, those with public insurance, a history of child protective services (CPS) involvement or abuse, an outpatient narcotic prescription for non-procedural pain management during pediatric care, a history of unscheduled hospitalization, emergency department (ED) visit, or at least one no-show visit during the final year in pediatric care, and prior cyclophosphamide therapy (p< 0.03). Gender, age at transfer, SLE disease duration, and income based on zip-code were not significantly related to development of ESRD or death. In logistic regression, public insurance, history of CPS involvement or abuse, and an unscheduled pediatric hospitalization were associated with development of ESRD or death (Table 1).
Of 114 patients for whom healthcare utilization data were available following final pediatric visit, 53% had a hospitalization in adult care. Time interval to first adult hospitalization was shorter for patients of Black race or Hispanic ethnicity, those with public insurance, a history of CPS involvement or abuse, an outpatient narcotic prescription for non-procedural pain management during pediatric care, a history of unscheduled hospitalization, ED visit, and no-show visit during the final year in pediatric care (p< 0.03) (Figure 2). In Cox regression analysis, a pediatric outpatient narcotic prescription was associated with shorter time to hospitalization while White or Asian race was associated with longer time to first hospitalization (p< 0.007).
Conclusion: Our findings indicate that efforts to improve transition outcomes among patients with cSLE should focus on high risk individuals in pediatric care, including those of Black race or Hispanic ethnicity, patients with public insurance, a history of CPS involvement or abuse, outpatient narcotic prescription for non-procedural pain management, and history of hospitalization, ED visit or no-show visit in the final year of pediatric care.
 Figure 1. Pediatric Factors Associated with ESRD or Death after Transfer to Adult Care
Figure 1. Pediatric Factors Associated with ESRD or Death after Transfer to Adult Care
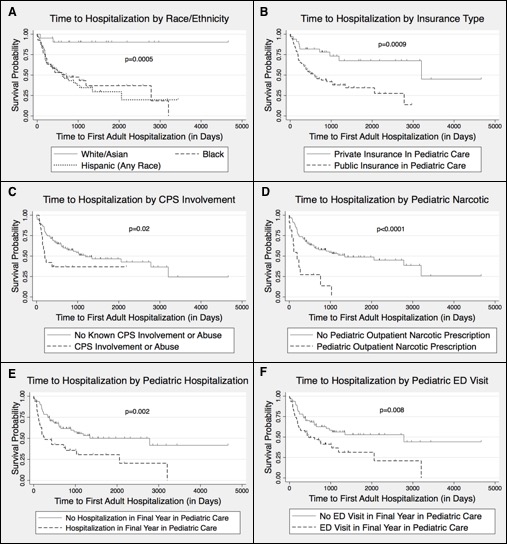 Figure 2. Time to Adult Hospitalization by Pediatric Factors
Figure 2. Time to Adult Hospitalization by Pediatric Factors
 Table 1. Stepwise Regression Models of Pediatric Predictors of Outcomes in SLE
Table 1. Stepwise Regression Models of Pediatric Predictors of Outcomes in SLE
To cite this abstract in AMA style:
Bitencourt N, Makris U, Solow E, Wright T, Bermas B. Predictors of Adverse Outcomes in Patients with Childhood-Onset Systemic Lupus Erythematosus Transitioning to Adult Care [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/predictors-of-adverse-outcomes-in-patients-with-childhood-onset-systemic-lupus-erythematosus-transitioning-to-adult-care/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-adverse-outcomes-in-patients-with-childhood-onset-systemic-lupus-erythematosus-transitioning-to-adult-care/
