Session Information
Date: Sunday, October 26, 2025
Title: (0554–0592) Spondyloarthritis Including Psoriatic Arthritis – Treatment Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Risk factors to identify patients who will develop a difficult-to-treat (D2T) psoriatic arthritis (PsA) are still lacking when initiating a first bDMARD. There are ongoing GRAPPA/EULAR definitions of D2T PsA. The primary endpoint of this work was to determine the risk factors for developing D2T PsA in patients initiating a first bDMARD using the definition from Philippoteaux et al [1]. The second objective was to determine the risk factors for developing refractory PsA in the same population.
Methods: A retrospective study was conducted at three secondary and tertiary centres in France and one tertiary centre in the United Kingdom. Patients with PsA aged 18 years or older who initiated b/tsDMARDs and had at least a five-year follow-up were included. D2T PsA was defined as failure of ≥ 2 b/tsDMARDs with different mechanisms of action, including TNF, IL-17, IL-23, and JAK inhibitors. Refractory PsA was defined as the failure of TNF, IL-17, IL-23, and JAK inhibitors. Patients with D2T PsA’s characteristics were compared with patients without D2T Patients with D2T PsA’s characteristics were compared with patients without D2T using logistic regression models adjusted for country (France vs. the United Kingdom). Factors significant at the 0.05 level were introduced into a multivariate logistic regression model also adjusted for country. The same methods were applied to compare patients with refractory PsA to those without refractory PsA. However, multivariate analysis was not performed due to limited sample size. The evolution of baseline characteristics was also assessed during four periods: before 1992, 1992 to 2002, 2003 to 2013, and 2014 to 2024.
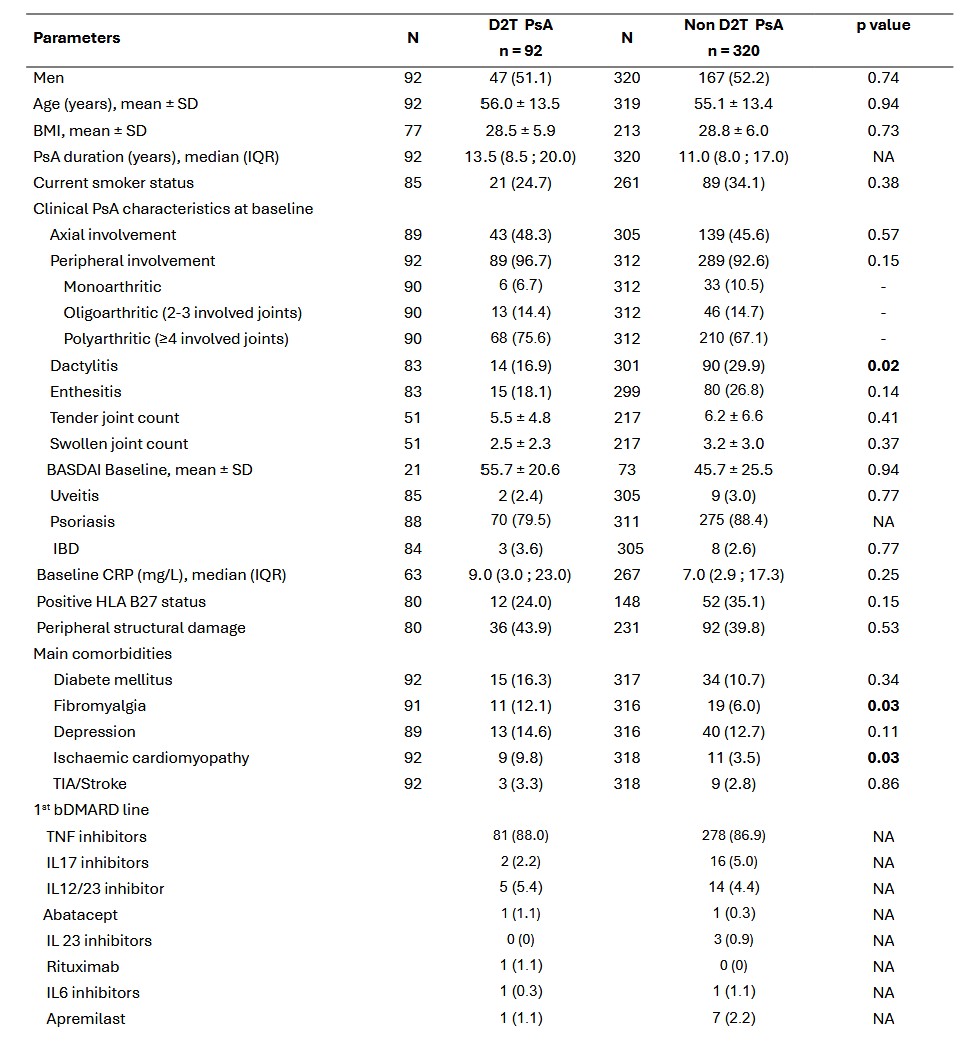
Results: Four hundred and twelve patients were included: 92 with D2T PsA (22.3%; 95% confidence interval [CI], 18.3-26.7) and 320 without D2T PsA (77.7%). The median disease duration was 12.0 (8.0; 18.5). Treatment trajectories of the patients were reported from the 1st to the 6th line (Figure 1). A higher proportion of patients with D2T PsA had dactylitis, fibromyalgia and ischaemic cardiomyopathy (Table 1). In multivariate analysis, fibromyalgia (OR = 2.62; 95% CI 1.09-6.28) and ischemic cardiomyopathy (OR = 2.95; 95% CI 1.04-8.36) were found to be risk factors for D2T PsA. On the contrary, dactylitis was a protective factor for D2T PsA (OR=0.49; 95% CI 0.26-0.94). The proportion of patients with peripheral structural damage, inflammatory bowel disease, uveitis, diabetes mellitus, and dyslipidaemia at baseline decreased over time, where the proportion of patients with axial structural damage, ischaemic cardiomyopathy, stroke, obesity, polyarticular PsA (i.e ≥ four involved joints) and dactylitis were stable over time (Figure 2). Fourteen patients (3.4%; 95% CI 1.9-5.6) were categorised as refractory. A refractory phenotype was associated with axial radiographic structural damage at baseline (OR = 5.65; 95% CI, 1.69-18.89).
Conclusion: In this retrospective binational study, fibromyalgia and ischaemic cardiomyopathy were found to be potential risk factors for D2T PsA, whereas dactylitis was a potential protective factor for D2T PsA. The prevalence of patients with refractory PsA was rare (< 5%) and was associated with axial radiographic structural damage at baseline.
Table 1 Baseline characteristics of patients with D2T PsA and those without PsA patients
Values are expressed as number (%) unless otherwise stated. BASDAI: Bath Ankylosing Spondylitis Disease Activity; bDMARD: biological disease modifying antirheumatic drug; BMI: body mass index; CRP: C-reactive protein; D2T: difficult-to-treat; HLA: human leukocyte antigen IBD: inflammatory bowel disease; IQR: interquartile range; N: number of available observations; NA: not applicable; PsA: psoriatic arthritis; SD: standard deviation; TIA: transient ischaemic accident; TNF:Tumour Necrosis Factor.
.jpg) Figure 1 Treatment trajectories from first to sixth line
Figure 1 Treatment trajectories from first to sixth line
.jpg) Figure 2 Evolution of phenotypes depending on the year of diagnosis
Figure 2 Evolution of phenotypes depending on the year of diagnosis
To cite this abstract in AMA style:
Goudot A, Hurtubise R, Robin E, Cadart L, Ramachandran R, Re F, Pascart T, Philippoteaux C, Flipo R, Coates L, Letarouilly J. Predictor Risk Factors For Developing Difficult-to-Treat Psoriatic Arthritis in Patients Initiating a First bDMARD: a Binational Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/predictor-risk-factors-for-developing-difficult-to-treat-psoriatic-arthritis-in-patients-initiating-a-first-bdmard-a-binational-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictor-risk-factors-for-developing-difficult-to-treat-psoriatic-arthritis-in-patients-initiating-a-first-bdmard-a-binational-study/