Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Anti-melanoma differentiation-associated gene 5 (MDA5) antibody is useful to predict mortality in patients with myositis–associated interstitial lung disease (ILD) because of high prevalence of rapidly progressive ILD, which is often refractory to conventional immunosuppressive treatment. In Japan, an intensive combination therapy consisting of corticosteroids (CS), calcineurin inhibitor, and intravenous cyclophosphamide, named the triple combo therapy, is widely used in patients with anti-MDA5-associated ILD anecdotally without evidence. A number of reports have shown that a group of anti-MDA5-associated ILD patients poorly respond to triple combo therapy. The aim of this study is to identify baseline characteristics that predict a poor response to triple combo therapy in patients with anti-MDA5-associated ILD, using a multicenter retrospective/prospective cohort JAMI, involving 497 incident cases of adult myositis-ILD.
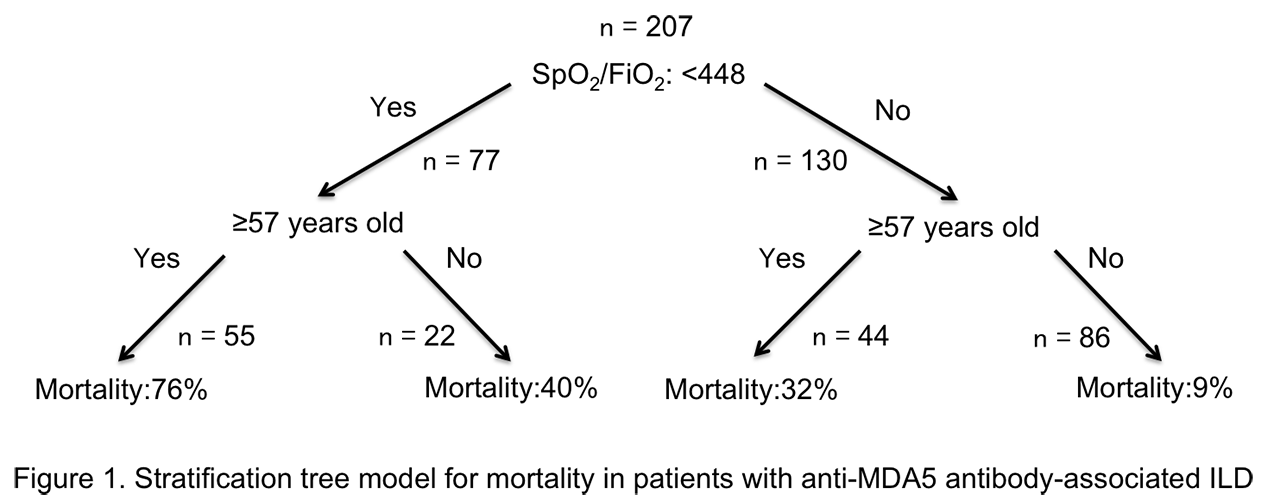
Methods: We selected 212 patients with anti-MDA5 from the JAMI database. First, baseline characteristics and treatment regimens were compared between survivors and non-survivors to identify factors associated with mortality using univariate analysis. We then conducted a multivariate logistic regression analysis to identify independent risk factors for mortality with stepwise selection method, in which explanatory variables were selected using backward deletion (P ≥ 0.15) and forward inclusion (P < 0.1). A stratification tree model was constructed based on the combination of risk factors. Finally, we compared survival rates between patients treated with initial triple combo therapy and those without, by selecting patients randomly using JMP®13 software (SAS Institute Inc., Cary, NC, USA) by matching the baseline risk stratification and additional treatment regimen such as CS pulse therapy. Cumulative survival rates were compared using log-rank test.
Results: Mean age at disease onset was 55, 136 (64%) were female, and median disease duration at entry was 2 months. 73 patients died due to respiratory insufficiency at median of one month after treatment introduction. Independent risk factors for mortality were older age (odds ratio [OR] 1.07, 95% confidence interval [CI] 1.04-1.12, P < 0.0001), and lower SpO2/FiO2 ratio (OR 0.98, 95%CI 0.96-0.99, P < 0.0001). Cut-off values that best discriminate survivors and non-survivors identified using ROC curve analysis included age of 57 years and SpO2/FiO2 ratio of 450. We successfully generated a stratification tree model for mortality (Figure 1). Patients older than 57 years with SpO2/FiO2 ratio < 450 at diagnosis had the worst outcome with mortality rate of 76%. Cumulative survival rates were comparable between patients treated with initial triple combo therapy and those without even after matching the baseline risk stratification and additional treatment regimen (Figure 2).
Conclusion: Age and SpO2/FiO2 ratio at diagnosis are independent predictors for mortality in patients with anti-MDA5-associated ILD. We failed to demonstrate superiority of triple combo therapy over conventional therapy even adjusting baseline risk factors, suggesting urgent need of other therapeutic regimen for this devastating condition.
To cite this abstract in AMA style:
Gono T, Masui K, Nishina N, Sato S, Kuwana M. Predictive Factors for Mortality in Anti-melanoma-associated Gene 5 Antibody-associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/predictive-factors-for-mortality-in-anti-melanoma-associated-gene-5-antibody-associated-interstitial-lung-disease/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictive-factors-for-mortality-in-anti-melanoma-associated-gene-5-antibody-associated-interstitial-lung-disease/