Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The ACC/AHA recommends preventive strategies for patients with a high predicted risk of atherosclerotic cardiovascular disease (CVD). RA patients are at higher risk for CVD events, yet the role of systemic inflammation and the influence of traditional CVD risk factors is unclear with respect to risk prediction in RA. A simple and accurate algorithm for predicting CVD event risk that includes systemic inflammation might help risk assessment for RA patients and optimize preventive care.
Methods: We derived a U.S. cohort of RA patients with multi-biomarker disease activity (MBDA) test results linked to Medicare claims data. Patients had to have ≥1 year baseline with Medicare coverage prior to the first MBDA test. Exclusions were past MI, PCI/CABG, stroke, or cancer. Follow-up ended at the earliest of 1) CVD event; 2) other than CVD cause of death; 3) loss of coverage; or 4) 12/31/2014. The composite CVD event comprised of incident MI, stroke or fatal CVD event, using validated algorithms. MBDA scores were grouped as low (<30), moderate (30-44), and high (>44). Other predictors included demographics, healthcare utilization, and comorbidities. Three separate models were developed using Cox regression. Model 1 included age, sex and race. Model 2 included age, sex race, 9 comorbidities and CVD medication classes, plus interaction terms. Model 3 included age, sex, and race plus categorized MBDA score. We calculated the net reclassification index (NRI) for model 2 and 3 compared to model 1. We also plotted the observed vs. predicted probability of CVD event for each model, with risk categorized as low (<7.5), moderate (7.5-<15) and high (≥15) per 1000 person-years based upon annualized ACC/AHA cutpoints.
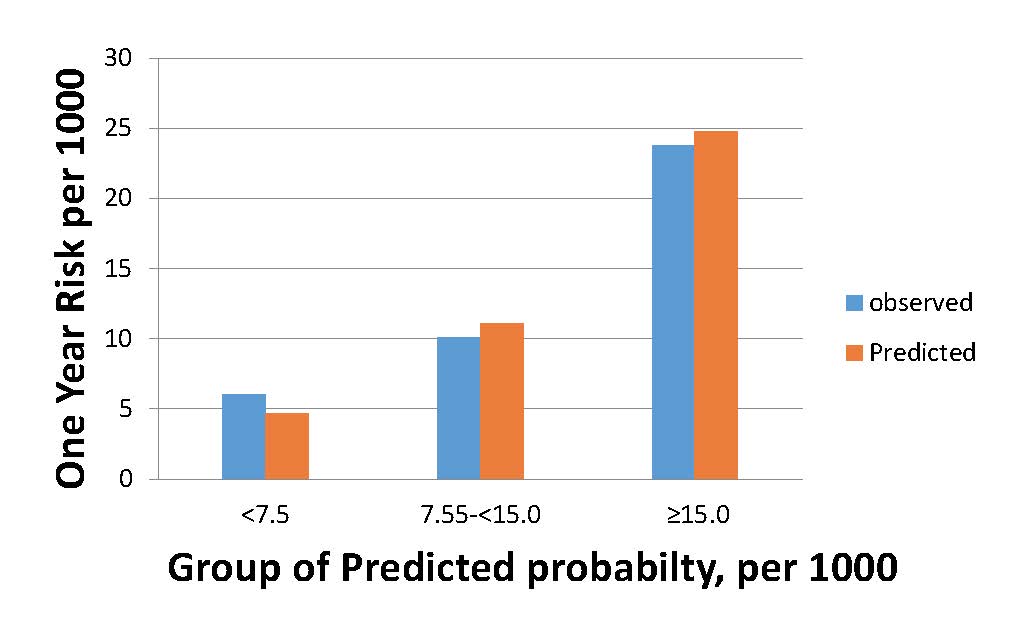
Results: A total of 15,757 RA patients were included; mean (SD) age 68.6(10.8) years, 80% female, 80% white. A total 209 CVD events occurred in 14,843 person years (1.41/100 py). The median (IQR) follow up time was 0.84 (0.41, 1.27) year. The maximum event time was at 2.7 year. All models had reasonable discrimination and calibration; model 3 was better than models 1 and 2 and observed vs predicted risk is shown (Figure). The sum of the absolute difference between observed and predicted probability was 0.56, 0.57 and 0.33 for models 1, 2 and 3 respectively. Compared to model 1, model 2 resulted in a positive overall NRI of 0.214 (non-event NRI=0.173, event NRI=0.041); model 3 resulted in positive overall NRI of 0.279 (non-event NRI=0.092, event NRI=0.187), consistent with more accurate CVD event classification.
Conclusion: Preliminary results from this analysis suggest that a simple algorithm consisting only of age, sex and race plus a multi-biomarker score can provide an accurate method to predict short term CVD risk in RA. Further validation with more extended time frames should improve the utility of this approach.
Figure: Observed vs. Predicted One-Year CVD Risk per 1000 person-years in RA Patients, using only Age, Sex, Race, and MBDA score (Model 3)
To cite this abstract in AMA style:
Xie F, Chen L, Yun H, Curtis JR. Prediction of Cardiovascular Events in Rheumatoid Arthritis Patients Using a Multi-Biomarker of Disease Activity [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/prediction-of-cardiovascular-events-in-rheumatoid-arthritis-patients-using-a-multi-biomarker-of-disease-activity/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prediction-of-cardiovascular-events-in-rheumatoid-arthritis-patients-using-a-multi-biomarker-of-disease-activity/