Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Vascular disease is of fundamental importance in the pathogenesis of scleroderma. Two major vascular complications in scleroderma patients that cause substantial morbidity and mortality are digital ulcerations (DU) and pulmonary hypertension (PH). The ability to predict which patients will develop these complications is poor in current clinical practice.
Methods: We conducted a prospective observational cohort study of 300 patients who were subsequently followed for at least a five-year period. Adult patients were included that met American College of Rheumatology criteria for scleroderma or have at least 3 of 5 features of the CREST syndrome. At baseline patients lacked evidence of pulmonary hypertension (PH) and were without current DU. At each visit the patient was examined for signs and symptoms of development of PH and DU. The primary outcomes were (1) pulmonary hypertension defined as a mean pulmonary artery pressure greater than or equal to 25 mm Hg obtained by right heart cardiac catheterization and (2) DU were defined as new onset of severe vascular compromise as evidenced by development of ischemic digital ulcerations, gangrene or digital loss. All classes of PH were modeled together in the primary analysis (pulmonary arterial hypertension (PAH), interstitial lung disease-associated PH) as these classes are not pathogenically mutually exclusive.
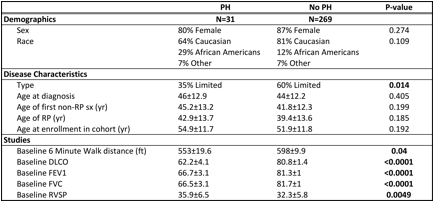
Results: The majority of the patients in the cohort (N=300) were middle-aged Caucasian females, with 13% of patients being male and 14% being African American. 58% of the patients had limited disease with an average disease duration of 10 ± 8.4 years from 1st non-RP symptom at study entry. Tables 1 & 2 show demographic data and baseline values for clinical tests by each of the individual outcomes. Patients who developed PH were more likely to have diffuse disease compared to patients without PH. Interestingly, baseline DLCO was lower in patients who develop both DU and PH. There was no difference in DU incidence in PH compared to non-PH groups (Fisher exact p=0.38).
Conclusion: We hypothesized that baseline echocardiographic and pulmonary function study parameters would be predictive of vascular outcomes. Our study demonstrates that the diffuse subtype and the distance walked at the baseline 6-minute walk test are predictive of developing PH, but not DU. We speculate that there may be unique pathophysiology that contributes to developing different vascular outcomes.
Table 1. Differences in Patient Characteristics by Pulmonary Hypertension Status 
Table 2. Differences in Patient Characteristics by Digital Ulcerations
To cite this abstract in AMA style:
Mecoli CA, Shah AA, Boin F, Wigley FM, Hummers LK. Predicting Vascular Complications in Systemic Sclerosis: A Prospective Cohort Study [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/predicting-vascular-complications-in-systemic-sclerosis-a-prospective-cohort-study/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predicting-vascular-complications-in-systemic-sclerosis-a-prospective-cohort-study/