Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Macrophage activation syndrome is a diagnosis along the spectrum of hemophagocytic lymphohistiocytosis (HLH) spectrum disorders. It is a rare, yet potentially fatal disease characterized by hyperferritinemia, coagulopathy and multisystem inflammation. Predictive biomarkers for outcomes in MAS are lacking and hence this study yearns to elucidate them. Activation of complement cascade and bacterial infection, causes a rise in the CRP whereas macrophage activation is represented by ferritin levels. These represent different immunological processes and are independent predictors of mortality in systemic inflammatory response.
Methods: We retrospectively reviewed 43 MAS patients admitted in our tertiary care centre, from the period of January 2021 to January 2022. All patients fulfilled the HLH 2004 diagnostic criteria or 2016 consensus criteria for MAS associated with systemic JIA, were included in this study. Our primary objective was to describe the clinical, etiological and laboratory profile of 43 consecutive cases of macrophage activation syndrome.
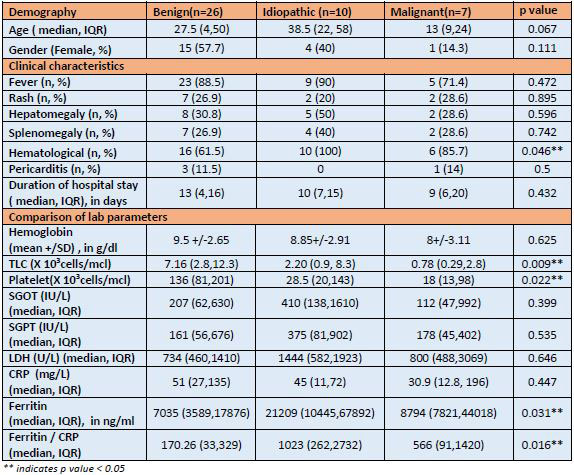
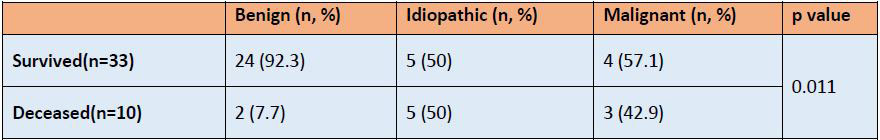
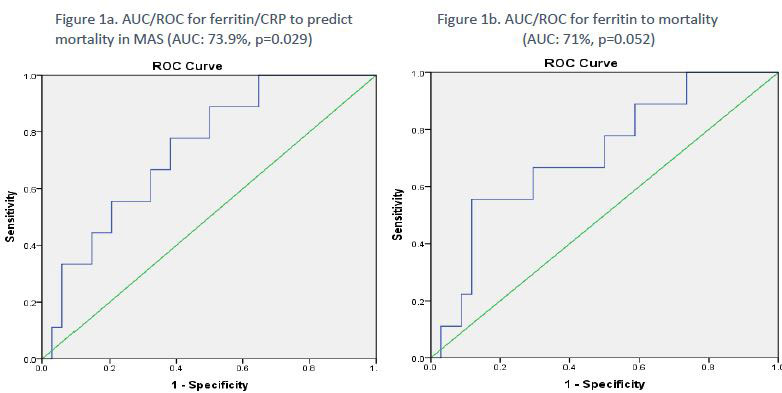
Demographic and clinical data, treatment and mortality at 6 weeks were analysed. Patients included a heterogeneous population including children and adults. They were broadly classified into MAS associated with benign disease, idiopathic HLH and malignancy associated HLH. Benign disease included underlying connective tissue disease, infections, Systemic JIA, Familial HLH, and Kikuchi disease. To test the statistical significance of the difference in the lab and clinical parameters with the diagnosis, Pearson Chi Square test was applied. ROC curve analysis was used to determine the cut-off values for ferritin and ferritin/CRP to predict mortality and diagnostic measures was computed. A p value of < .05 was considered to be statistically significant.
Results: A total of 43 (20 females) patients with MAS were included. Twenty six (60.46%) patients had an underlying benign disease, 10(23%) were idiopathic and 7(16%) had an underlying hematological malignancy. Majority of patients had fever (86%) and hematological manifestations (75%). The total leukocyte count, platelet, Ferritin/CRP ratio and ferritin showed a statistically significant difference between groups. Median values for CRP was also low in patients with malignancy, however this difference was not statistically significant. There was a statistically significant (p=0.011) association with mortality at 6 weeks and underlying diagnosis. The variables that showed a significant association with mortality at 6 weeks were ferritin (Fig. 1a) and ferritin/CRP ratio (Fig. 1b). The cut off determined for ferritin was 7511 (Sensitivity: 89%, Specificity: 41%) and ferritin/ CRP was 204.5(Sensitivity: 89%, Specificity: 50%).
Conclusion: In this study, MAS was most often caused secondary to a benign disease. The most common presentation was fever with cytopenias. Ferritin levels more than 7511 and ferritin/ CRP levels more than 204.5 was associated with higher mortality. These findings emphasize the need for early referral of patients with suspected macrophage activation syndrome, particularly patients with high ferritin and ferritin and CRP ratio, irrespective of etiology of MAS.
To cite this abstract in AMA style:
Madan S, Balan S, CHALAKKARAYIL BHAGAVALDAS M, DR S, Rath S, Thattil J, Shahul A, Kartha N. Predicting Outcomes in Macrophage Activation Syndrome (MAS): A Retrospective Study on 43 Consecutive Patients with MAS [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/predicting-outcomes-in-macrophage-activation-syndrome-mas-a-retrospective-study-on-43-consecutive-patients-with-mas/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predicting-outcomes-in-macrophage-activation-syndrome-mas-a-retrospective-study-on-43-consecutive-patients-with-mas/