Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Total Hip (THA) and total knee arthroplasty (TKA) are cost-effective procedures that improve the health-related quality of life for patients with advanced symptomatic joint damage, including patients with rheumatoid arthritis (RA). However, increasing utilization has led to marked increase in cost with inpatient costs representing the largest proportion of expenditures for TKA. For this reason, it is important for cost containment efforts to address length of stay (LOS). Preoperative opioid usage has been associated with increased LOS and postoperative complications in osteoarthritis (OA) patients. Patients with RA have a longer LOS after THA/TKA than OA patients, yet the factors contributing to LOS, including preoperative opioid use, have not been investigated.
Methods: We retrospectively reviewed data from a prospectively collected cohort of 252 RA patients undergoing either THA or TKA. Demographics, RA characteristics, medications, and disease activity were systematically collected pre-operatively. Disease activity was measured utilizing the DAS28 and CDAI, PROMs included HOOS/KOOS and MDHAQ, and ESR, CRP, and serologies were drawn pre-operatively. Baseline characteristics were summarized using descriptive statistics and compared using Chi-squared, Fisher’s exact test, or two-sample t-test or Wilcoxon rank-sum test as appropriate. Linear Regression analysis was performed to explore the relationship between LOS (log-transformed) and predictors. The final multivariate model was constructed through backward selection among predictors that were found statistically significant (p< 0.05) in the univariate analysis.
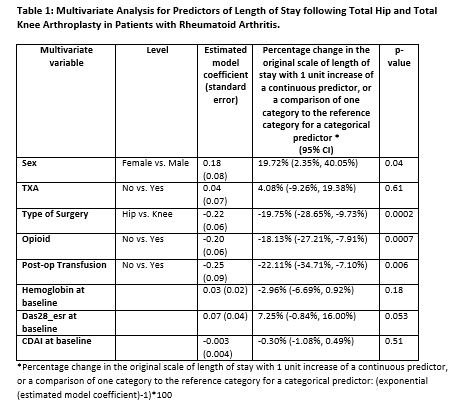
Results: RA cases were predominantly women (83%), with median disease duration (14.1 +/-12 years), and moderate disease activity (mean DAS28= 3.7±1.3, CDAI=18.4±10.9). 240(95%) cases had LOS data available. 88 (37%) patients were taking opioids pre-operatively. The mean LOS was 3.4±1.5 days with those undergoing THA having a LOS of 3.1±1.6 and TKA with a LOS of 3.7±1.4. In the univariate analysis, post-operative transfusion (p=0.01), baseline DAS 28 (p=0.02), sex (p=0.001), BMI (p=0.03), Employment status (p=0.04), type of surgery (p< 0.001), opioid usage (p=0.001), duration of surgery (p=0.01), HOOS/KOOS baseline pain score (p=0.01), HOOS/KOOS baseline function score (p=0.003), duration of disease (0.03), baseline MD-HAQ (p=0.01), baseline ESR (p=0.03) were significantly associated with extended LOS. The multivariate analysis revealed several factors that impact LOS. LOS was decreased for patients who underwent THA (p=0.002), male gender (p=0.04), did not have a post-op transfusion (p=0.006) and did not take opioids pre-operatively (p=0.0007) (Table 1).
Conclusion: Patients who receive a post-operative transfusion, undergo knee surgery, women, and increased opioid usage were associated with increased length of stay. While gender and surgical type are non-modifiable risk factors, pre-operative optimization should focus on transfusion risk factors and pre-operative opioid reduction. We recommend that patients undergo pre-operative opioid cessation counseling, and multimodal pain management should be used peri-operatively to reduce opioid usage.
To cite this abstract in AMA style:
Morse K, Heinz N, Abolade J, Wright-Chisem J, Russell L, Zhang M, Mirza S, Orange D, Figgie M, Sculco P, Goodman S. Pre-Operative Opioid Usage Increases Length of Stay for Rheumatoid Arthritis Patients Undergoing Total Hip Arthroplasty and Total Knee Arthroplasty [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/pre-operative-opioid-usage-increases-length-of-stay-for-rheumatoid-arthritis-patients-undergoing-total-hip-arthroplasty-and-total-knee-arthroplasty/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pre-operative-opioid-usage-increases-length-of-stay-for-rheumatoid-arthritis-patients-undergoing-total-hip-arthroplasty-and-total-knee-arthroplasty/