Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Renal disease is common in ANCA-associated vasculitis (AAV) and one of the goals of early treatment is to maximize renal function recovery. Corticosteroids are a cornerstone of induction treatment. However, the optimal dosing and weaning schedule is not known. The objectives of this study are to: 1) Describe practice variation in corticosteroid use in treatment of pediatric AAV with renal disease; 2) Assess for associations between baseline patient characteristics and corticosteroid dose at the time of diagnosis; and 3) Explore whether any variation in corticosteroid use at diagnosis is associated with outcomes at 12 months.
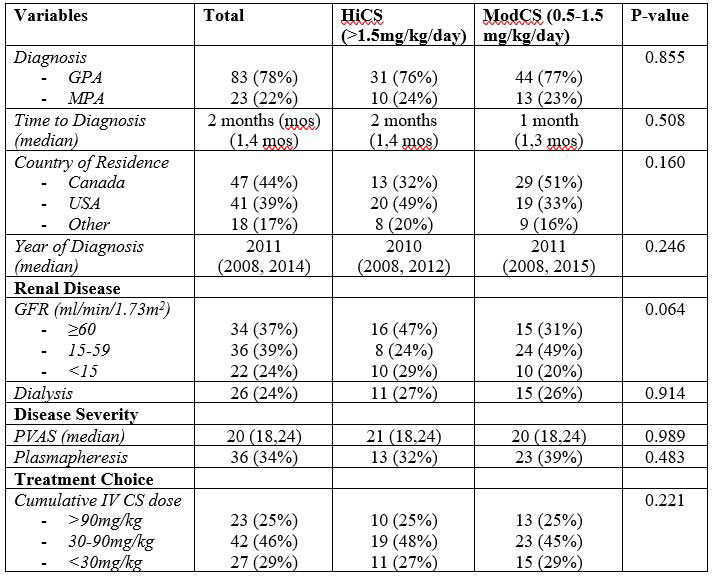
Methods: Patient data was obtained from an international pediatric vasculitis registry – PedVas. Patients followed for at least 12 months with AAV and biopsy confirmed pauci-immune glomerulonephritis were included. Patients’ baseline characteristics such as dialysis requirement, glomerular filtration rate (GFR) and pediatric vasculitis activity score (PVAS) were examined for associations with the oral corticosteroid dose initiated at diagnosis. Outcomes analyzed for association with oral corticosteroid dose at diagnosis included GFR at 12 months, and the ability to wean to < 0.2mg/kg/day of oral corticosteroid. Statistical analysis was conducted using the Chi-squared test for proportions and the Mann-Whitney U Test. Results: 106 patients were included in total. 83 (78%) patients were diagnosed with GPA, and 24 (21%) had MPA. 28 (26%) patients required dialysis at diagnosis, and 36 (34%) received plasmapheresis as part of induction treatment. 41 (38.7%) received >1.5mg/kg/day of oral corticosteroid (Hi-CS) and 57 (53.8%) received 0.5-1.5mg/kg/day of oral corticosteroid (Mod-CS) at diagnosis. No significant difference was found between oral CS dosing groups with regards to baseline patient characteristics (Table 1). Additionally, no associations were found between oral corticosteroid dose at diagnosis and 12 month outcomes such as renal function (Table 2).
Conclusion: Corticosteroid use in pediatric AAV with renal disease is highly variable, and with no associations between baseline patient characteristics and oral corticosteroid dose, it is unclear what guides physicians’ use of corticosteroid at diagnosis. Furthermore, the results suggest that patient outcomes at 12 months were not improved for those treated with higher oral corticosteroid doses at diagnosis. This study highlights the need for prospective studies to further explore optimal corticosteroid dosing strategies in pediatric AAV.
To cite this abstract in AMA style:
Chen A, Mammen C, Guzman J, Cabral D, Morishita K. Practice Variations in Treatment of Pediatric Anti-neutrophil Cytoplasmic Antibody (ANCA)-associated Vasculitis (AAV) with Renal Disease [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/practice-variations-in-treatment-of-pediatric-anti-neutrophil-cytoplasmic-antibody-anca-associated-vasculitis-aav-with-renal-disease/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/practice-variations-in-treatment-of-pediatric-anti-neutrophil-cytoplasmic-antibody-anca-associated-vasculitis-aav-with-renal-disease/