Session Information
The 2020 Pediatric Rheumatology Symposium, originally scheduled for April 29 – May 2, was postponed due to COVID-19; therefore, abstracts were not presented as scheduled.
Date: Saturday, May 2, 2020
Title: Poster Session 3
Session Type: ACR Abstract Session
Session Time: 4:15PM-5:15PM
Background/Purpose: Pediatric Rheumatology (PR) is a young and still evolving subspecialty. In addition to traditional rheumatic diseases, there has been an increased prevalence of emerging inflammatory syndromes in children. These patients are often critically ill requiring care in an intensive care unit (ICU). There is a paucity of data on PR involvement in this acute period. We assessed practice patterns of pediatric critical care medicine (PCCM) specialists for consulting PR.
Methods: This was an IRB-approved exploratory survey of PCCM faculty at a quaternary children’s hospital that was collected from April-June 2018. It included questions about clinical exposure to rheumatic conditions, triggers for consultation, and challenges encountered in the ICU. Study data were collected using REDCap and descriptive statistics were analyzed.
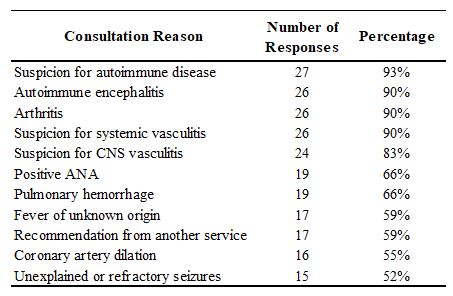
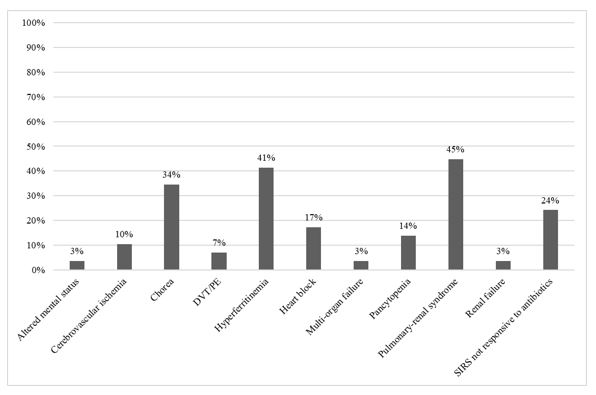
Results: A total of 29 (73%) PCCM faculty completed the survey. Median year since fellowship completion was 7 and median year at current institution was 8 (range 0-23 years). Nearly all respondents have cared for patients with traditional rheumatic disorders such as GPA, MAS, Kawasaki disease, SLE, APS, JDM, systemic JIA, and MCTD. 90% always consult PR for patients admitted with known rheumatic diagnoses. 66% reported that they have observed an increased frequency of novel systemic inflammatory conditions seen in the ICU over the last decade. The most common reasons for PR consultation were undifferentiated abnormalities in neurologic, hematologic, pulmonary, renal, or musculoskeletal organ systems (Table 1). From a rheumatology perspective, there were several physiologic manifestations that had lower than expected consultation rates (Figure 1). These included altered mental status, cerebrovascular ischemia, thrombotic events, chorea, heart block, hyperferritinemia, multi-organ failure, pancytopenia, pulmonary-renal syndrome, renal failure, and systemic inflammatory response syndrome not responsive to antibiotics.
Conclusion: PCCM faculty had extensive exposure to traditional rheumatic conditions, autoinflammatory syndromes and undefined systemic inflammation; however, several phenotypes associated with systemic rheumatic disease had lower than expected consult rates. These data help provide information on CCM practice patterns and educational opportunities for rheumatologists to pursue to help ensure timely collaboration for early identification and improved outcomes for patients with rheumatic diseases.
To cite this abstract in AMA style:
Rammel J, Thammasitboon S, Coss Bu J, Muscal E. Practice Patterns for Consulting Pediatric Rheumatology in a Large Pediatric Intensive Care Unit [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 4). https://acrabstracts.org/abstract/practice-patterns-for-consulting-pediatric-rheumatology-in-a-large-pediatric-intensive-care-unit/. Accessed .« Back to 2020 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/practice-patterns-for-consulting-pediatric-rheumatology-in-a-large-pediatric-intensive-care-unit/