Session Information
Date: Sunday, November 7, 2021
Title: Pediatric Rheumatology – Clinical Poster II: SLE, JDM, & Juvenile Scleroderma (0764–0785)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Prior studies have demonstrated alarming health disparities in adult patients with SLE, including higher disease severity and activity among Hispanic and Black patients. Pediatric studies have demonstrated similar racial disparities, including associations between Hispanic and Black race and end stage renal disease, increased health utilization, and death among hospitalized patients. Importantly, prior studies do not focus on modifiable risk factors of socioeconomic status (SES), such as income level, particularly important as exiting poverty demonstrated potential reversibility of disease damage in an analysis of the Lupus Outcomes Study. Our study aims to use the most recent iteration (2016) of the Kids’ Inpatient Database (KID) – the largest all-payer pediatric inpatient care database in the U.S. – to investigate the relationship between income level and hospital length of stay (LOS) via cross-sectional analysis.
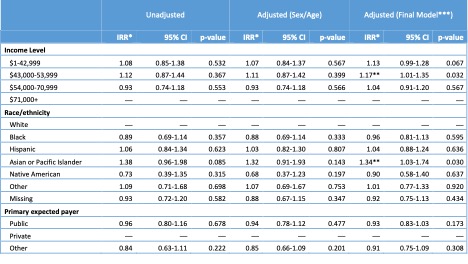
Methods: SLE hospitalizations were identified for children ages 2-20 by a primary ICD-10 diagnosis code of M32. Those with neonatal lupus (ICD-10 M32.8) were excluded. Baseline characteristics were compared by income level (Quartile 1, 2, 3, and 4) using descriptive statistics (ANOVA and Pearson’s chi-squared exact tests, as appropriate). Negative binomial regression was used to analyze the effect of income level (by median income for zip code divided into quartiles) on length of stay unadjusted, then adjusted for sex and age, and finally adjusted for other covariates of interest (race/ethnicity, primary payer status) and confounders (APRDRG severity of hospitalization, presence of severe lupus features, and location/teaching status of hospital). Using this adjusted model, a marginal mean length of stay was calculated at each income quartile.
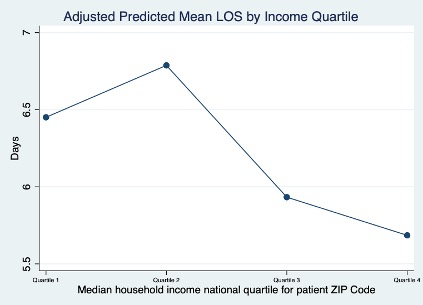
Results: A total of 1,586 primary lupus hospitalizations were identified (Table 1). The mean age at admission was 16 with a female predominance (84%). This cohort represented a diverse patient population (36% Black, 27% Hispanic, 8% Asian/Pacific Islander vs 14% White) with higher proportions of minority populations in the lower compared to upper income quartiles (i.e. Black 50% in Quartile 1 & 31% in Quartile 2 vs 27% in Quartiles 3 & 4). Private insurance coverage was more common in the highest income quartile (62% in Quartile 4 vs 26% in Quartile 1). In unadjusted analysis, income level was not associated with increased LOS though adjusted analysis did demonstrate an association with prolonged increased length of stay at the 2nd income level (IRR 1.17, p-value 0.032 – Table 2). Adjusted mean length of stay was higher than the mean for those with lower income levels (Quartile 1 and 2 – Figure 1).
Conclusion: Lower income level may be associated with prolonged LOS among children hospitalized with SLE though this association was only significant at the 2nd level of income quartile. This may reflect that those of lowest income are supported by resources not available to others in poverty who miss strict guidelines for assistance, such as housing support. Future work will include income as a predictor of readmissions and recurrent ED visits.
(*IRR = Incidence rate ratio;
**Achieving statistical significance at p-value <0.05;
***Multivariate negative binomial regression model adjusted for age, sex, hospital region, location/teaching status of hospital, presence of severe lupus features, APRDRG Severity Index + primary payer/income level and/or race/ethnicity)
(*Multivariate negative binomial regression model adjusted for age, sex, race/ethnicity, insurance type, hospital region, location/teaching status of hospital, presence of severe lupus features, and APRDRG Severity Index)
To cite this abstract in AMA style:
Soulsby W, Lawson E, Pantell M. Poverty and Length of Stay in Children Hospitalized with Pediatric Systemic Lupus Erythematosus: An Analysis of the 2016 Kids’ Inpatient Database [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/poverty-and-length-of-stay-in-children-hospitalized-with-pediatric-systemic-lupus-erythematosus-an-analysis-of-the-2016-kids-inpatient-database/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/poverty-and-length-of-stay-in-children-hospitalized-with-pediatric-systemic-lupus-erythematosus-an-analysis-of-the-2016-kids-inpatient-database/