Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Posttraumatic Stress Disorder (PTSD), a complex psychiatric disorder that can result from experiencing or witnessing a traumatic event, such as an accident, assault, or death. We aimed to assess the prevalence of PTSD symptoms at the onset of the COVID-19 pandemic among individuals with or without systemic autoimmune rheumatic disease (SARD) diagnoses, given the increased stress those with SARDs may have experienced given their immunosuppression.
Methods: In May 2020, at the start of the COVID-19 pandemic, we invited 6,681 patients of a large multihospital system who had opted in to research opportunities (including 378 with ≥ 2 ICD 9/10 prior PTSD codes) to complete the Brief Trauma Questionnaire and the Posttraumatic Stress Disorder Checklist (PCL-5). The Brief Trauma Questionnaire and the PCL-5 are previously validated questionnaires that can identify individuals with probable PTSD. Diagnoses for prior PSTD, SARD, anxiety, depression, and adjustment disorders were identified using ICD-9/10 billing code algorithms. Survey responses were analyzed using univariable t-tests to identify differences between SARDs and non-SARDs subjects. We used multivariable logistic regression to identify potential predictors of PCL-5 positivity, an indication for PTSD, at the time of survey distribution.
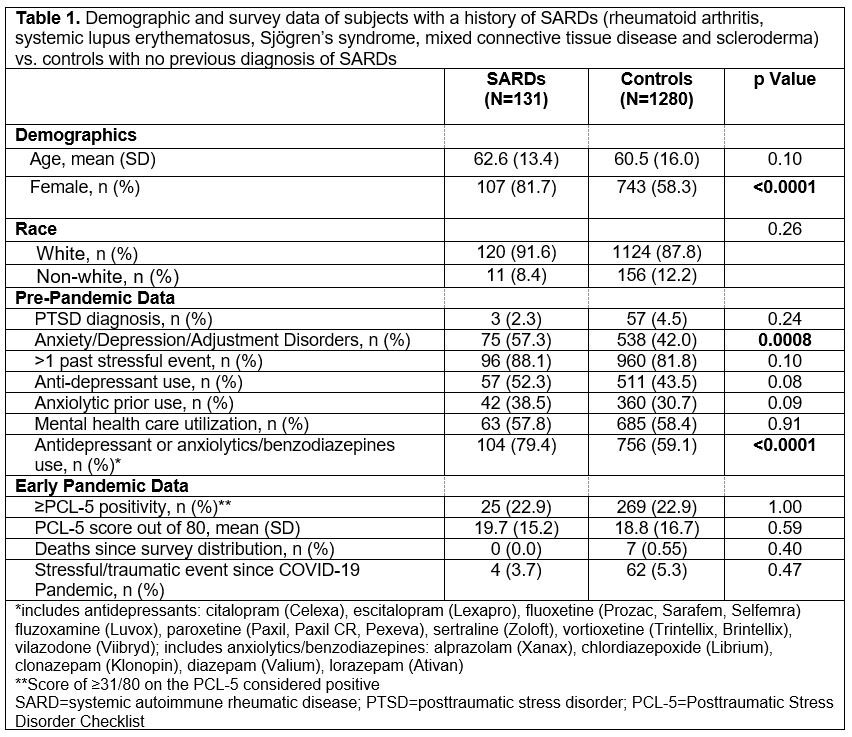
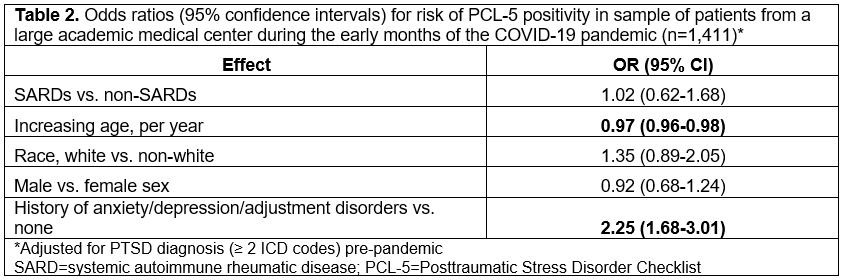
Results: We received 1,411 complete and unique responses (21% response rate) between 5/2020 and 9/2021, with most responses received in late May to early June 2020. Of these respondents, 60 had a history of PTSD prior to the pandemic and 131 had a prior history of a SARD (Table 1). In the univariable analysis, the SARDs population was significantly more female (p< 0.0001) and had a higher baseline prevalence of anxiety, depression, and adjustment disorders (p=0.0008) than respondents without SARDs. In the early pandemic, there were no significant differences in PCL-5 scores (p=0.59), PCL-5 positivity (p=1.00), or traumatic events (p=0.47) between those with and without a SARDs diagnosis. Upon adjusting for pre-pandemic PTSD diagnoses, we found younger age (OR=0.97, 95% CI [0.96, 0.98] per increasing year) and history of anxiety, depression, or adjustment disorder (OR=2.25, 95% CI [1.68, 3.01]) to be the most significant predictors of PCL-5 positivity during the early pandemic (Table 2).
Conclusion: While SARDs was not a significant predictor of new onset PTSD symptoms, we found that younger individuals and those with a history of baseline anxiety, depression, or adjustment disorders, which were more common pre-pandemic among those with SARDs, were more likely to screen positive on the PCL-5 during early COVID-19 pandemic. The lack of increased PTSD symptoms in SARDs vs. non-SARDs populations suggests that during the early months of the pandemic, SARDs patients may not have been at higher risk for new PTSD symptoms.
To cite this abstract in AMA style:
Ellrodt J, Oakes E, Kubzansky L, Koenen K, Guan H, Costenbader K. Posttraumatic Stress Disorder Symptoms in Systemic Autoimmune Rheumatic Disease Patients During the Early COVID-19 Pandemic [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/posttraumatic-stress-disorder-symptoms-in-systemic-autoimmune-rheumatic-disease-patients-during-the-early-covid-19-pandemic/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/posttraumatic-stress-disorder-symptoms-in-systemic-autoimmune-rheumatic-disease-patients-during-the-early-covid-19-pandemic/