Session Information
Date: Monday, November 11, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster II: Treatments, Outcomes, & Measures
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Post-traumatic stress disorder (PTSD) is associated with worse outcomes among U.S. Veterans with rheumatoid arthritis (RA) in addition to reduced medication adherence in other chronic disorders. This study examined the association between PTSD and DMARD discontinuation, accounting for comorbidity and other potential confounders that may impact this relationship.
Methods: VA administrative data were used to define unique dispensing episodes of methotrexate (MTX), self-injectable TNF inhibitors (TNFi), other DMARDs, and prednisone for Veterans with a prior diagnostic code for RA. Discontinuation was defined as a lapse in drug refill >90 days. Patient characteristics and diagnosis codes were linked to treatment courses. Patient characteristics were analyzed based on the first dispensing episode of each unique DMARD. Some patients switched TNFi’s over time and thus accounted for multiple dispensing episodes. Diagnosis codes (using a “lifetime” lookback) were used to delineate RA patients into 3 mutually exclusive groups: PTSD (with or without depression/anxiety), depression and/or anxiety without PTSD, and none of the aforementioned diagnoses. Multivariate Cox proportional hazards models were used to evaluate associations between psychiatric diagnoses and time to DMARD discontinuation. Covariates included age, sex, race (Black vs. White), calendar year (2005-2009 vs. 2010-2014), BMI, other DMARDs, Rheumatic Disease Comorbidity Index (RDCI), CRP, anti-CCP status, RA duration >5 years, diabetes, hypertension, CHF, history of malignancy, and current smoking status.
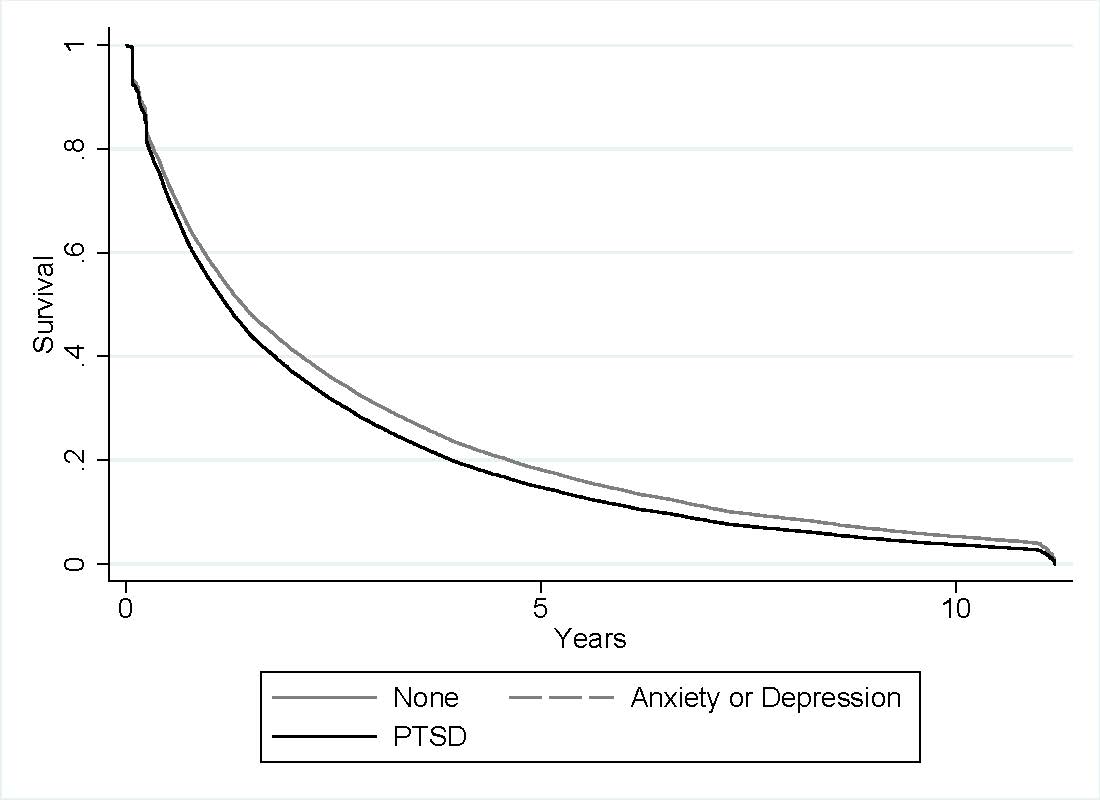
Results: There were 15,082 dispensing episodes of MTX in 15,082 unique patients and 8,412 dispensing episodes for TNFi in 7,092 unique RA patients. Patients were predominantly Caucasian (74% MTX, 77% TNFi) and male (88% MTX, 87% TNFi). Median drug survival was 1.30 years (95% CI 1.27-1.35) for MTX and 1.18 years (95% CI 1.13-1.24) for TNFi. Comorbid PTSD was seen in 20% of those initiating MTX and 22% of those initiating TNFi. Depression and/or anxiety (without PTSD) was seen in 23% of those initiating MTX and 27% of those initiating TNFi. After adjusting for covariates, PTSD was associated with a greater likelihood of discontinuing both MTX [HR 1.12 (1.07,1.18) p< 0.001; Figure 1] and TNFi [HR 1.16 (1.09,1.23) p< 0.001; Figure 2]. Risk of discontinuation in depression/anxiety without PTSD was comparable to that seen in PTSD for both MTX [HR 1.12 (1.07,1.17) p< 0.001] and TNFi [HR 1.14 (1.08,1.21) p< 0.001].
Conclusion: Veterans with RA and a diagnosis of PTSD, depression, or anxiety discontinued DMARDs sooner than those without these diagnoses, even after accounting for a number of other factors. Rates of discontinuation were similar for those with PTSD compared to those with depression and/or anxiety alone and were similar between MTX and TNFi. PTSD, anxiety, and depression may contribute to lower persistence of RA therapy due to non-adherence, apparent lack of response, or a greater incidence of adverse events.
-Note that PTSD and Anxiety/Depression groups have significant overlap in this figure-
-Note that PTSD and Anxiety/Depression groups have significant overlap in this figure-
To cite this abstract in AMA style:
Desilet L, Baker J, England B, Michaud K, Barton J, Mikuls T. Post-Traumatic Stress Disorder, Depression, Anxiety and Persistence of Methotrexate and TNF Inhibitors in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/post-traumatic-stress-disorder-depression-anxiety-and-persistence-of-methotrexate-and-tnf-inhibitors-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/post-traumatic-stress-disorder-depression-anxiety-and-persistence-of-methotrexate-and-tnf-inhibitors-in-patients-with-rheumatoid-arthritis/