Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Inflammation at vertebral corners on MRI has been shown to predict development of syndesmophytes in patients with AS. However, it is unclear at a patient level whether a positive spine MRI for inflammation identifies patients at higher risk for radiographic progression and whether this is also associated with the degree of spinal inflammation. We used the SPARCC MRI spine score to assess whether the proposed cut-off of ≥2 for positive spine MRI and the absolute score are predictive of radiographic progression.
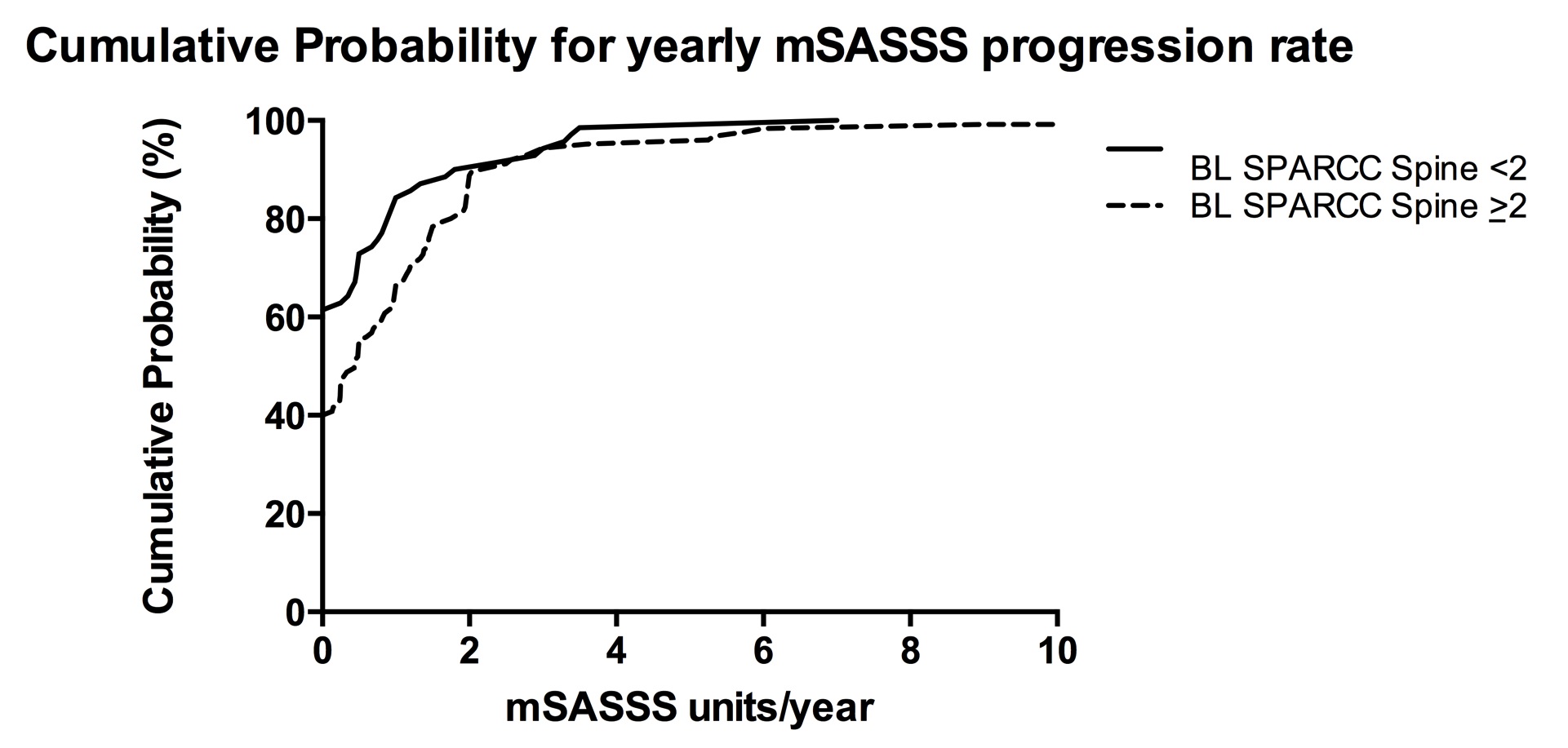
Methods: Spinal inflammation was scored blinded to time point (baseline, 2 years) using the SPARCC spine score by two readers and an adjudicator using pre-specified rules for adjudication. MRI scans were assessed from a prospective cohort of 195 AS patients (mean age 40.3 years, mean symptom duration 16.6 years, 59% on anti-TNF) followed for mean 2.3 years. Two readers and an adjudicator independently scored pairs of radiographs (baseline, 2 years) from the same patients using the mSASSS. Radiographic progression was compared in patients with and without positive spine MRI (SPARCC ≥2 or <2) and the degree of spinal inflammation at baseline (absolute SPARCC score) was compared in patients with and without radiographic progression (mSASSS >0 or =0) using Mann-Whitney and cumulative probability. Multivariate regression analyses included variables significant in univariate analyses (age, sex, symptom duration, CRP, baseline mSASSS) and treatment.
Results: Radiographic progression was significantly greater in those with positive spine MRI (p=0.004) (figure), and especially in patients who only received non-biologic therapy (p=0.006). Baseline SPARCC spine inflammation scores were significantly higher in those who developed radiographic progression compared to those without (14.5 vs 8.7, p=0.002). Positive spine MRI and the degree of spinal inflammation score were both significantly associated with radiographic progression in multivariate analysis (β=0.26 (p=0.019) and β=0.006 (p=0.036), respectively).
Conclusion: Both a positive spine MRI for inflammation and the degree of spinal inflammation are significantly associated with radiographic progression in patients with AS.
Disclosure:
W. P. Maksymowych,
None;
S. Wichuk,
None;
Z. Zhao,
None;
P. Chiowchanwisawakit,
None;
R. Lambert,
None;
S. Pedersen,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/positive-spine-mri-for-inflammation-predicts-radiographic-progression-in-patients-with-ankylosing-spondylitis/