Session Information
Date: Tuesday, November 12, 2019
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Patient Preferences, Beliefs, & Experiences
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Flare activity or worsening symptoms are not well defined for myositis. This analysis characterizes PM and DM flares from the patient perspective and reports the corresponding disability and rates for emergency department or urgent care visits and hospitalizations.
Methods: An online survey was conducted with volunteer patients recruited from The Myositis Association and Johns Hopkins Myositis Center. Survey questions included sociodemographics, flare symptoms, Health Assessment Questionnaire Disability Index (HAQ-DI) and HAQ-Pain index, Work Productivity and Activity Impairment (WPAI), myositis related emergency department and urgent care (ED/UC) visits and hospital admissions during the past year. Flare frequency was assessed with two sequential questions, “Have you ever had a flare or worsening myositis symptoms?” if yes, “How many times in the past 12 months?”.
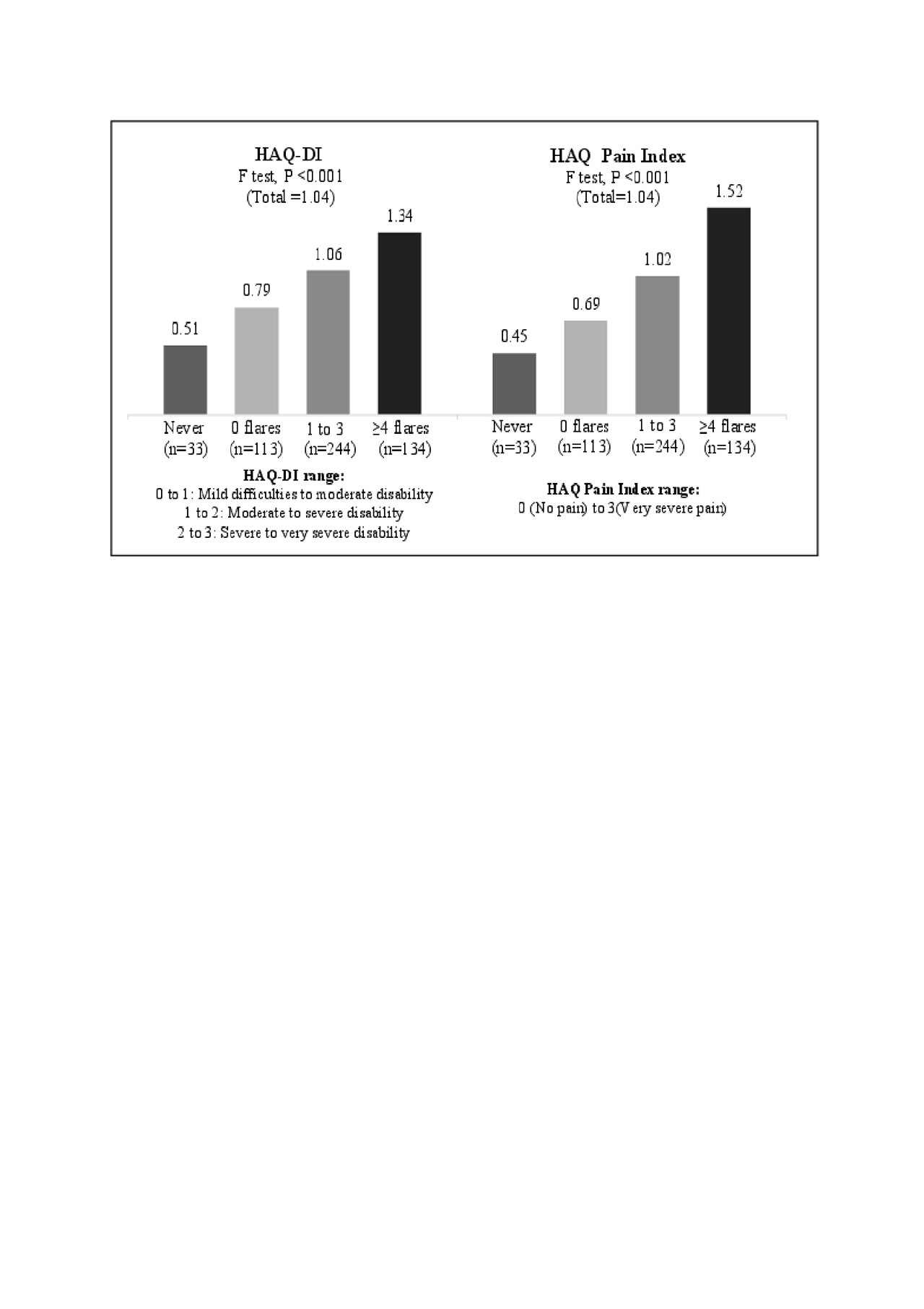
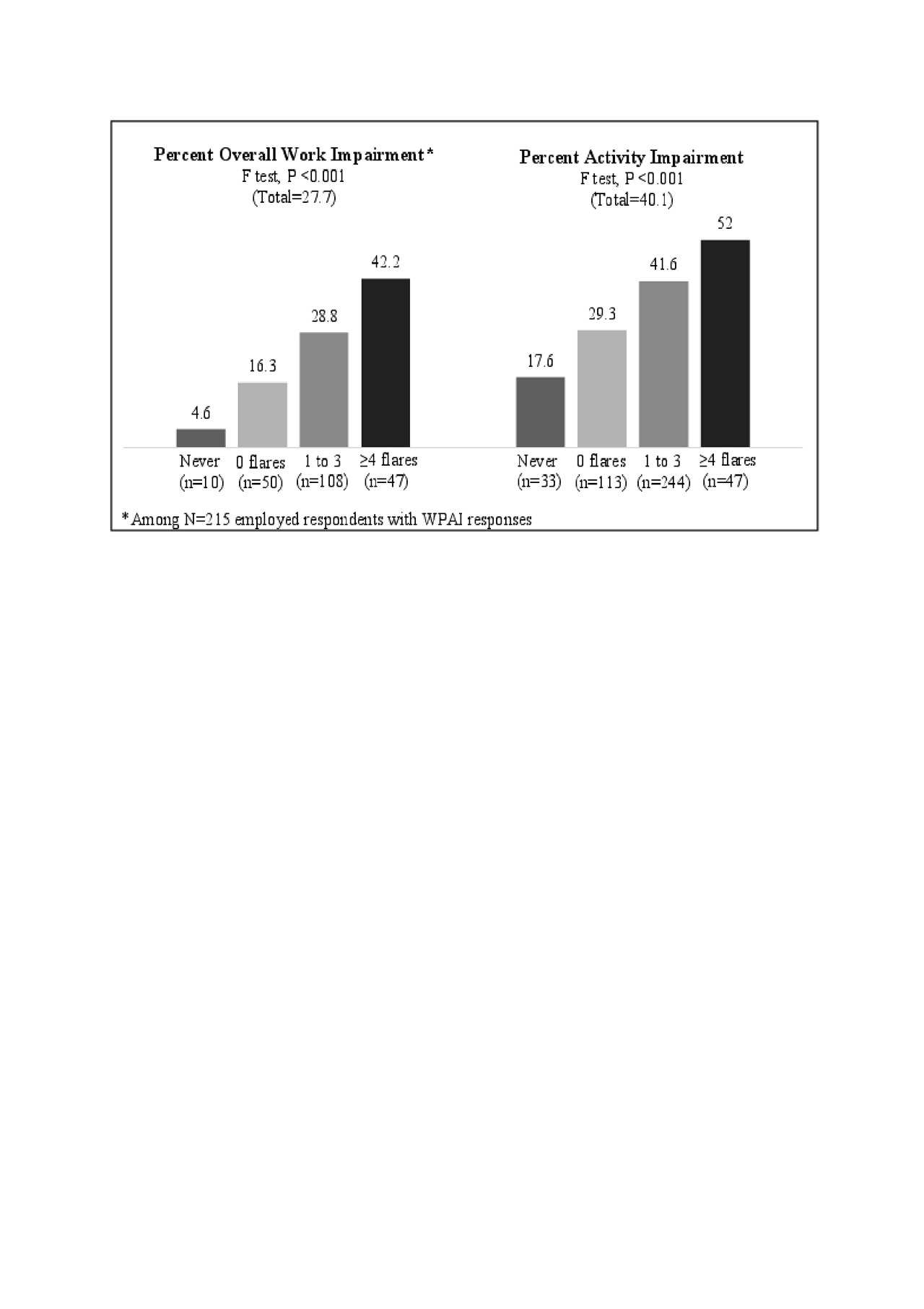
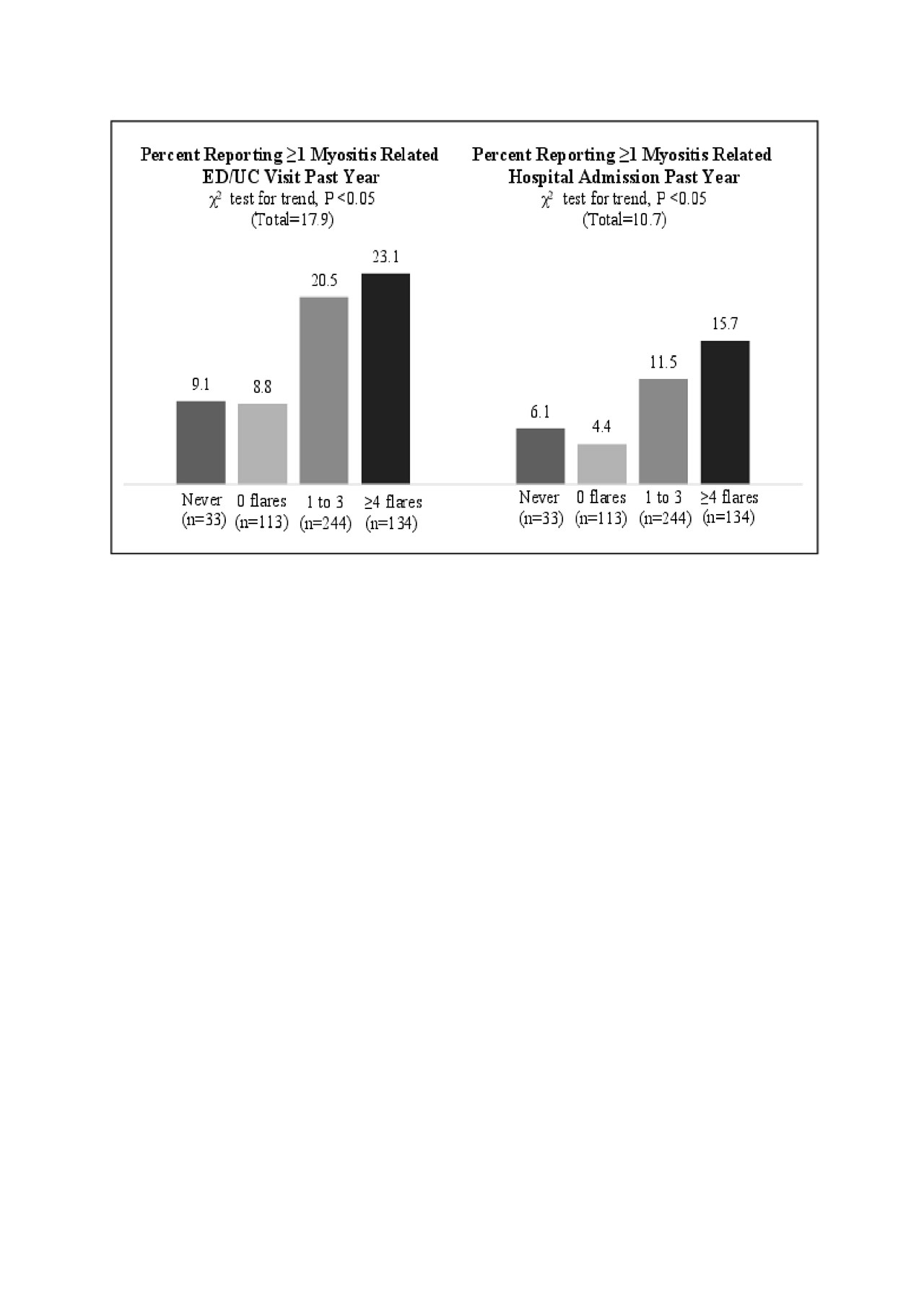
Results: A total of 564 patients with self-reported diagnoses of PM (n=243) or DM (n=321) completed the survey between December 2017 and May 2018 (86.3% Caucasian, 78.2% female, 42.9% employed, mean age 56). There were 524 who recalled periods with or without worsening symptoms or flares (demographic profile similar to total sample) and those individuals are reported on here. There were 33 (6.3%) that reported never experiencing a flare, 113 (21.6%) reported 0 flares in the past year, 244 (46.6%) reported 1-3 flares, and 134 (25.6%) reported 4 or more flares in the past year. The pattern of flare frequency was similar for PM and DM respondents. Among those with past year flares or periods of worsening symptoms (n=378) the most common symptoms were muscle weakness (83%), extreme fatigue or exhaustion (78%), muscle pain/discomfort (64%), trouble climbing stairs (62%), trouble standing from a seated position (50%), and skin rash (45%). Dysphagia occurred for 27%. Increasing flare frequency was associated with greater mean HAQ-DI (F=17.653, P < .001), HAQ-Pain (F=28.291, P < .001) (Figure 1), greater mean percent of WPAI activity impairment (F=20.109, P < .001) and for the employed, greater mean percent of missed work time (F=2.716, P < .05), as well as greater impairment at work (F=8.242, P < .001), and overall work impairment (F=9.933, P < .001) (Figure 2). Percent with one or more past year myositis related ED/UC visits were found to be related to flare frequency (χ2=11.634, P < .05). The percent with one or more myositis related hospital admissions was also associated with flare frequency (χ2=9.03, P < .05) (Figure 3).
Conclusion: PM/DM-related flares or worsening symptoms are common, with 72% of respondents reporting one or more flare occurrence in the past year. Exacerbations of muscle weakness and fatigue were the most common flare symptoms, and flare frequency was associated with greater disability, more pain, more overall work impairment, and more activity impairment. Past year ED/UC visits and hospital admissions were also more likely to occur as flare frequency increased. Higher frequency of patient-reported flares may serve as a marker of worsening physical functioning and intensifying health care needs, and therefore suggests their importance in the clinical assessment of patients with PM/DM.
To cite this abstract in AMA style:
Christopher-Stine L, Kelly W, Wan G, Kobert L, Reed M. Polymyositis (PM) and Dermatomyositis (DM) Symptom Flares and Associated Impact from the Patient Perspective [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/polymyositis-pm-and-dermatomyositis-dm-symptom-flares-and-associated-impact-from-the-patient-perspective/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/polymyositis-pm-and-dermatomyositis-dm-symptom-flares-and-associated-impact-from-the-patient-perspective/