Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Polymyositis (PM)/ Dermatomyositis (DM) is a chronic immune-mediated myositis characterized by relapses that can lead to frequent hospitalizations. There is a scarcity of national population-based studies on PM)/DM readmissions in the United States (US). In this study, we aim to describe the rates, reasons for readmissions, and characteristics of readmissions for adults hospitalized for PM/DM in the United States (US).
Methods: We analyzed the 2018 Nationwide Readmissions Database (NRD). It includes nested and weighted discharge data for 60% of the total US population from 28 states. These data are stratified in clusters to produce national estimates. The NRD captures admissions on a calendar-year basis (for this study, from January 1 to December 31, 2018) without links to the following or preceding year, which is why index admissions during December, October to December, and July to December were excluded for the 30-, 90-, & 180-day readmission analysis, respectively. Therefore, index hospitalizations from January to November, January to September, and January to June were included in the 30-, 90- and 180-day readmissions analysis, respectively.
We included index hospitalizations for all adult DM/PM patients (aged ≥18 years) with a principal diagnosis of PM/DM using ICD-10 code “M33”. The principal diagnosis is the main reason for hospitalization. We excluded elective and traumatic readmissions. Readmission was calculated as the percentage of patients readmitted within a time frame over index hospitalizations that were discharged alive. Using a “rank” command in STATA, the most common specific principal diagnosis of readmissions was outlined. Chi-square tests were used to compare baseline characteristics between readmissions and index hospitalizations. STATA, 16 was used for analysis. Since NRD contains de-identified patient data, Institutional Review Board (IRB) review was not sought.
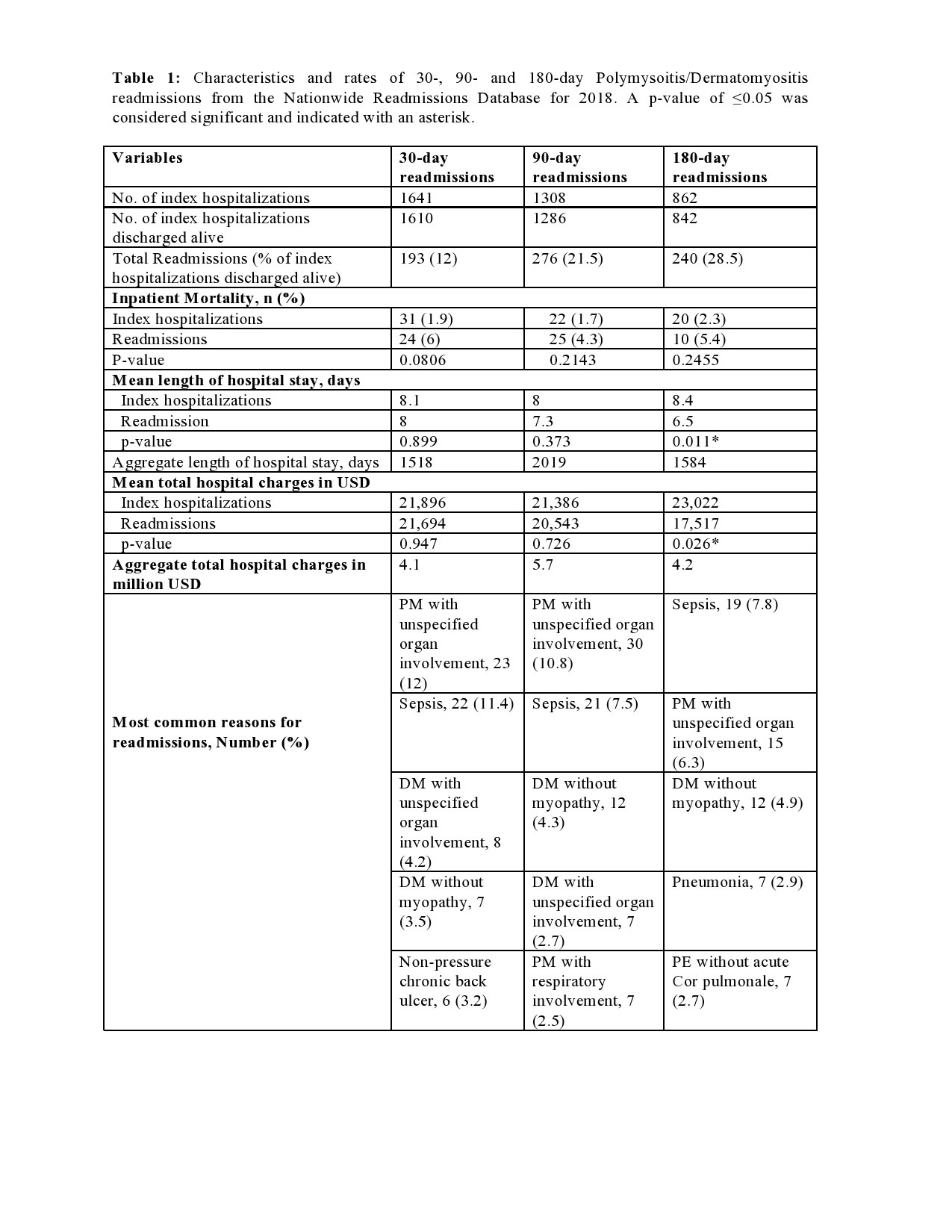
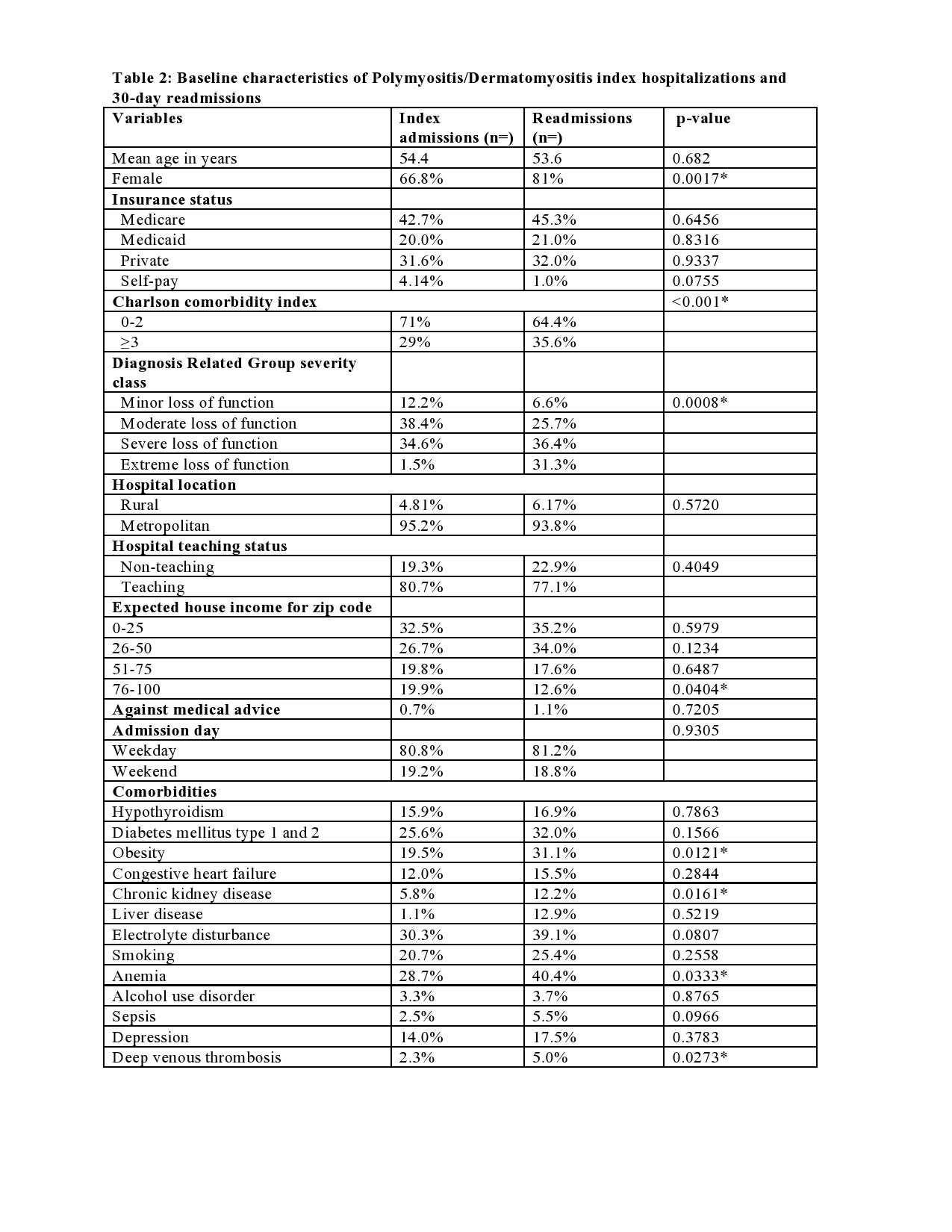
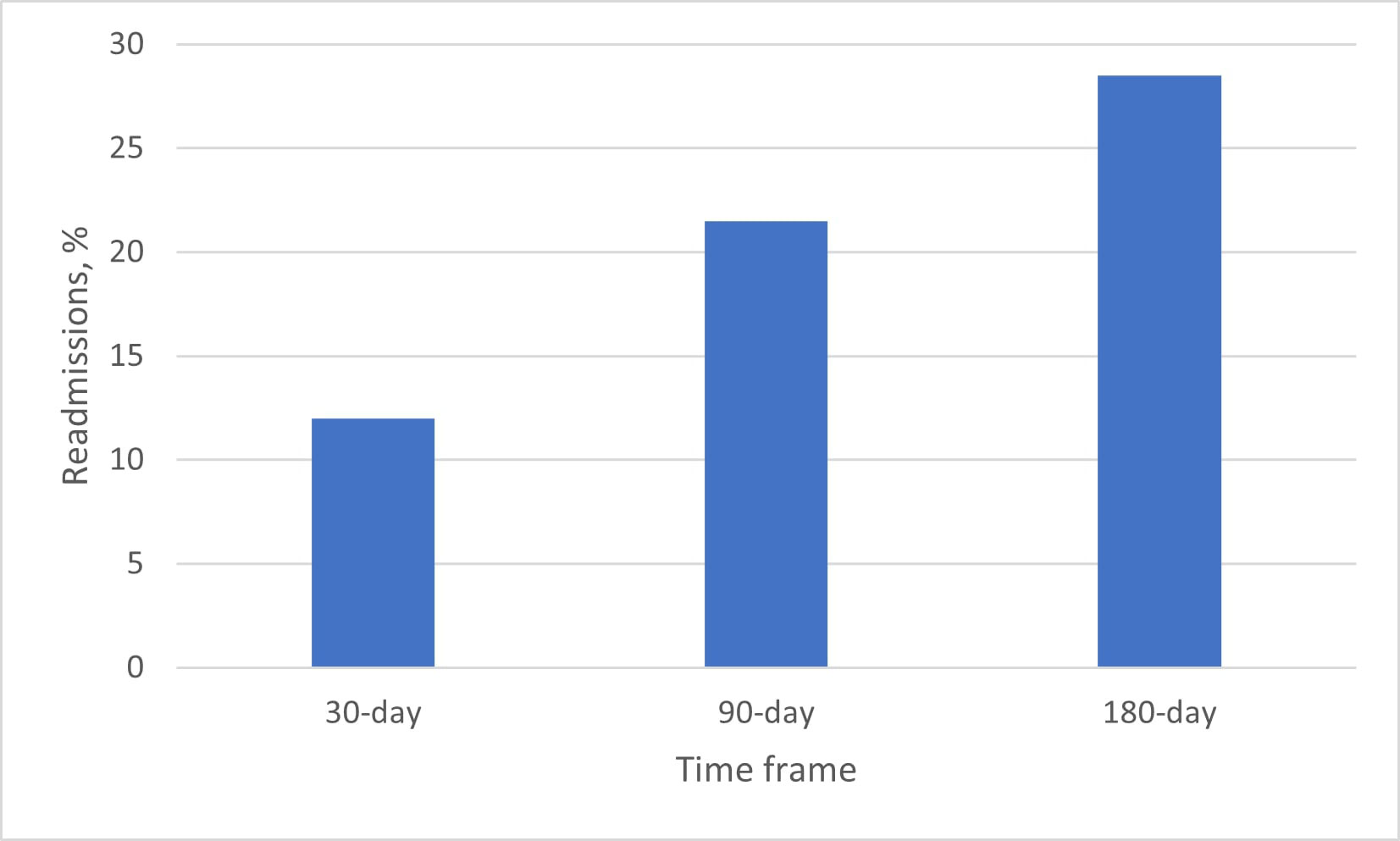
Results: A total of 1610, 1286, and 842 index hospitalizations with a principal diagnosis of PM/DM, that were discharged alive, were included in the 30-, 90- and 180-day readmission analysis respectively. Among these, 193 (12%), 276 (21.5%), and 240 (28.5%) were readmitted within 30, 90 and 180 days, respectively. PM with unspecified organ involvement and sepsis were the most common reasons for reasons across the 3 timeframes. 30-day readmissions were responsible for an aggregate of 4.1 million US dollars in total hospital cost and 1518 hospital days in 2018. Compared to index hospitalizations, 30-day readmissions were more likely to be females, have higher Charlson comorbidity index scores, severe-extreme loss of function, have a secondary diagnosis of obesity, chronic kidney disease (CKD), anemia, and Deep venous thrombosis (DVT).
Conclusion: Close to a third of PM/DM hospitalized patients are readmitted within 180 days. Readmissions constitute a significant economic burden to the health care system. PM and sepsis are the main reasons for readmissions. Readmissions have a higher comorbidity burden compared to index hospitalizations.
Readmission, % was calculated as the percentage of patients readmitted within a time frame over index hospitalizations that were discharged alive.
To cite this abstract in AMA style:
Edigin E, Trang A, Kannayiram S, Osuorji C, Hino C, Eseaton P, Anighoro S, Manadan A, Downey C. Polymyositis/Dermatomyositis Readmissions: Analysis of the Nationwide Readmission Database [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/polymyositis-dermatomyositis-readmissions-analysis-of-the-nationwide-readmission-database/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/polymyositis-dermatomyositis-readmissions-analysis-of-the-nationwide-readmission-database/