Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: We previously reported on difficult to treat Rheumatoid Arthritis (RA) in nearly 1600 patients treated with biologic (b) or target synthetic (ts) DMARDs including failure or were intolerant to all classes, i.e. what we termed poly-refractory RA (1).Here, we sought to characterise this further, by exploring whether there is an underlying inflammatory drive underpinning this response, by utilizing ultrasound.
Methods: We reviewed electronic medical records of all D2TRA and identified 40 patients with poly-refractory RA. In addition to clinical assessment, we performed musculoskeletal ultrasonography (US) of clinically swollen joints. Patients were divided into two groups according to the presence or absence of US synovitis, respectively Persistent Inflammatory Refractory RA (PIRRA) and Non-inflammatory Refractory RA (NIRRA). US synovitis was considered as the presence of both greyscale and power Doppler grades of at least 1. Univariate analyses were performed to differentiate the two groups’ characteristics.
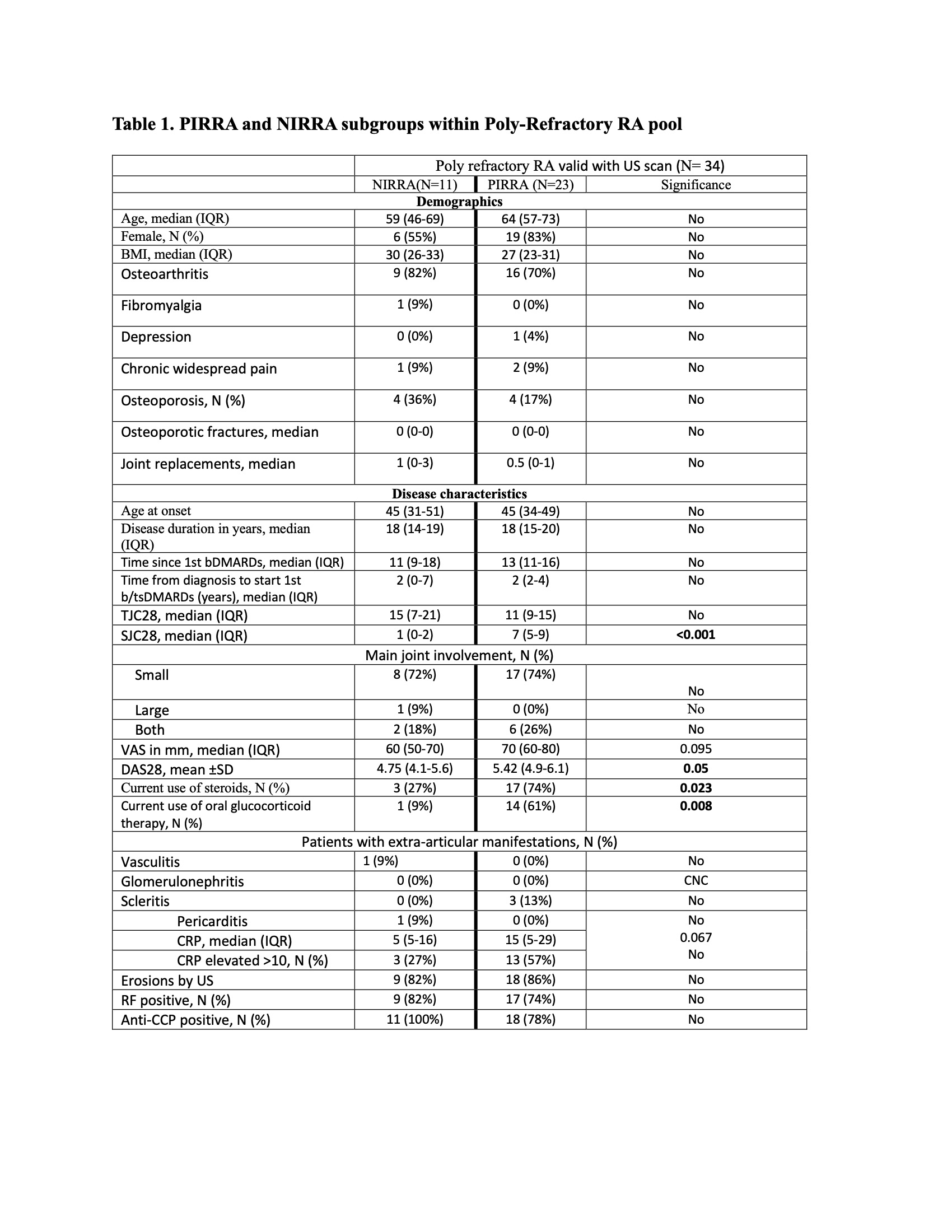
Results: Only 40 out of 1591 patients with poly-refractory RA representing only 2.5% of cases. Of these, 34 (85%) had a recent US. 3/34 died and 3/34 were lost to follow-up from our clinic. 23/34 (67.6%) had US synovitis and therefore had PIRRA, while 11/34 (32.4%) with no US synovitis were classified as NIRRA, with baseline characteristics of both grops described in Table 1. When compared to NIRRA, PIRRA poly-refractory patients had significantly higher SJC (7 vs 1, p < 0.001) and, as expected, DAS-28-CRP scores (5.42 vs 4.75, p = 0.05), as well as higher need for corticosteroids to control their symptoms (61% vs 9%, p = 0.008). CRP levels were numerically but not significantly higher in the PIRRA group (median 15 vs 5mg/L, p = 0.067). The NIRRA group had a higher BMI, that may have impacted on CRP levels, and contained more fibromyalgia patients.
Conclusion: Poly-Refractory RA represented only 2.5% of RA cases under b/tsDMARDs and at least one-third of those patients had no signs of active inflammation on US. Patients that had exhausted all available b/tsDMARD options, the NIRRA group, with objective evidence of inflammation comprised only 1.5% of RA.
References:
1- David P et al. EULAR 2023. Supplementary
To cite this abstract in AMA style:
David P, Di Matteo A, Hen O, Dass S, Marzo-Ortega H, Emery P, Saleem B, McGonagle D. Poly-Refractory Rheumatoid Arthritis: All B/tsDMARD Classes Exhausted – An Uncommon Disease Subset with Distinct Inflammatory and Non-inflammatory Phenotypes [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/poly-refractory-rheumatoid-arthritis-all-b-tsdmard-classes-exhausted-an-uncommon-disease-subset-with-distinct-inflammatory-and-non-inflammatory-phenotypes/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/poly-refractory-rheumatoid-arthritis-all-b-tsdmard-classes-exhausted-an-uncommon-disease-subset-with-distinct-inflammatory-and-non-inflammatory-phenotypes/