Session Information
Session Type: Abstract Session
Session Time: 5:00PM-6:00PM
Background/Purpose: Type 1 interferons (IFN-1) are major drivers of disease activity in systemic (SLE) and cutaneous lupus erythematosus (CLE). Plasmacytoid dendritic cells (pDCs) are the major producers of IFN-1 during viral infection. Therefore, pDCs have been hypothesized to be the primary IFN-1 producing cell in lupus. IFN-1 production by pDCs has not been extensively studied due to reliance on interferon gene signatures as a proxy for IFN-1 levels as well as a reliance on pDCs from healthy controls for in vitro studies. However, it has been known that pDCs are reduced in the circulation in SLE and have also been more recently shown to have an exhausted phenotype, suggesting that pathogenic pDCs may be located in the end organs.
Methods: Well characterized CLE patients were recruited from a prospective database. We performed imaging mass cytometry on archived treatment naïve CLE skin (n=48) and a subset were also used for mRNA in situ hybridization. Fresh 4mm punch biopsies (n=3) and blood (n=4) were obtained from CLE patients and healthy controls (n=3) for multiplexed flow cytometry or cytometry by time of flight (CyTOF).
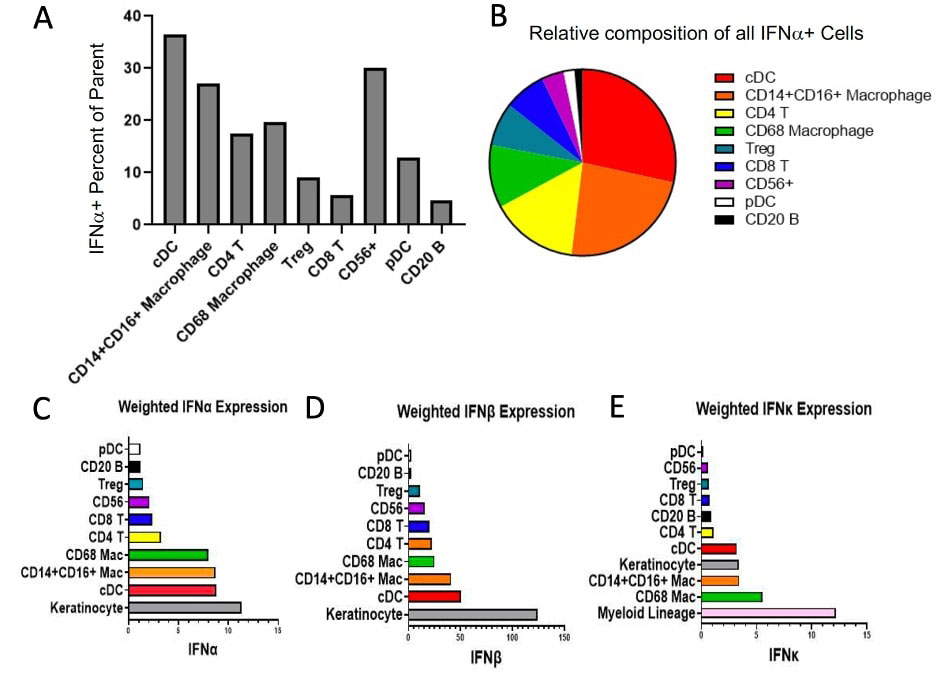
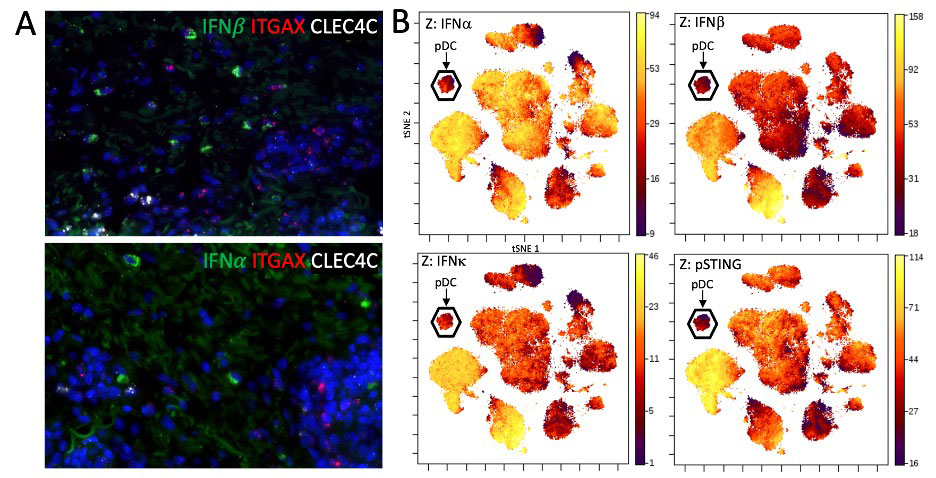
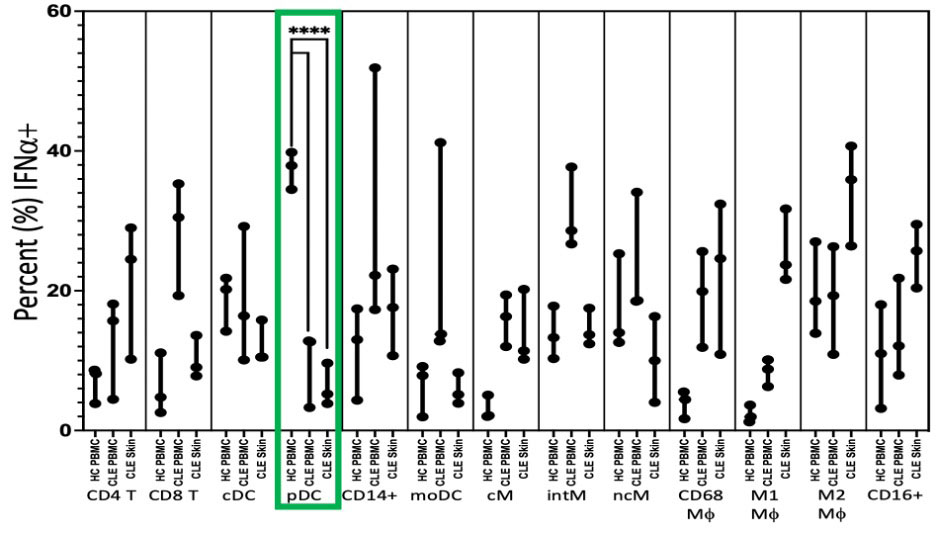
Results: In lesional CLE skin, only 8.5% (IQR 0.0-22.22) of pDCs were IFNa+. Across all CLE biopsies, pDCs were the second lowest contributor of absolute IFNα+ cells (Median 1; IQR 0-4.5), with B lymphocytes being the smallest contributor. Classic dendritic cells (cDCs) and macrophages (Mφ) were the largest relative and absolute contributors of IFNα in CLE. For IFNβ, only 16.7% of pDCs were positive, compared to 60.7% of CD14+CD16+ Mφ. pDCs were also the second lowest contributors of IFNβ+ cells (Median 1; IQR 0-7), with B lymphocytes again being the lowest. IFN-1 mRNA was detected in ITGAX (CD11c) positive cDCs but we did not identify colocalization of pDC-specific gene, CLEC4C (BDCA2), and IFN-1 mRNA. Flow cytometry on leukocytes eluted from fresh lesional biopsies showed a median of 5.2% of pDCs were positive for IFNα (IQR 3.85 – 9.64) which was significantly lower than the median of 37.9% of HC PBMC pDCs (34.5 – 39.8) (p< 0.0001). In comparison, other leukocytes in CLE skin displayed greater positivity for IFNα such as CD4 T cells (Median, IQR) (24.5%, 10.2 – 29), CD14+ cells (17.6%, 10.7 – 23.1), Classical Monocytes (CD14++CD16-) (11.4%, 10.2 – 20.2), Intermediate Monocytes (CD14++CD16+) (13.7%, 12.4 – 17.5), CD68+ Macrophages (24.6%, 10.9 – 32.4), M1 Macrophages (CD68+CD163-) (23.7%, 21.6 – 31.7), M2 Macrophages (CD68+CD163+) (35.9%, 26.4 – 40.7), and CD16+ cells (25.7%, 20.4 – 29.5). Further verification using a Z-axis overlay of intracellular markers on tSNE plots of immune cell clusters identified by CyTOF confirmed low expression of IFN-1and the interferogenic pathway, phosphorylated stimulator of interferon genes (pSTING), in the pDCs.
Conclusion: Taken together, these findings suggest pDCs may not play the central role in CLE as major IFN-1 producers and myeloid cells are larger contributors of IFN-1 in numbers and as a percent. pDCs may have a pathogenic role in CLE through IFN-1-independent mechanisms.
To cite this abstract in AMA style:
Vazquez T, Kodali N, Diaz D, Patel J, Keyes E, Sprow G, Sharma M, Ogawa-Momohara M, Grinnell M, Dan J, Werth V. Plasmacytoid Dendritic Cells Are Not Major Producers of Type 1 Interferons in Cutaneous Lupus [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/plasmacytoid-dendritic-cells-are-not-major-producers-of-type-1-interferons-in-cutaneous-lupus/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/plasmacytoid-dendritic-cells-are-not-major-producers-of-type-1-interferons-in-cutaneous-lupus/