Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Long-term management of rheumatoid arthritis (RA) relies on disease-modifying antirheumatic drugs (DMARDs), including conventional synthetic (csDMARDs), biologic (bDMARDs), and targeted synthetic (tsDMARDs). About 40% of patients do not respond to first-line csDMARDs, and they require more expensive bDMARDs or tsDMARDs. Equitable access to these treatments is a significant concern in the U.S. We examined racial and ethnic disparities in DMARD utilization among a nationally representative cohort of RA patients.
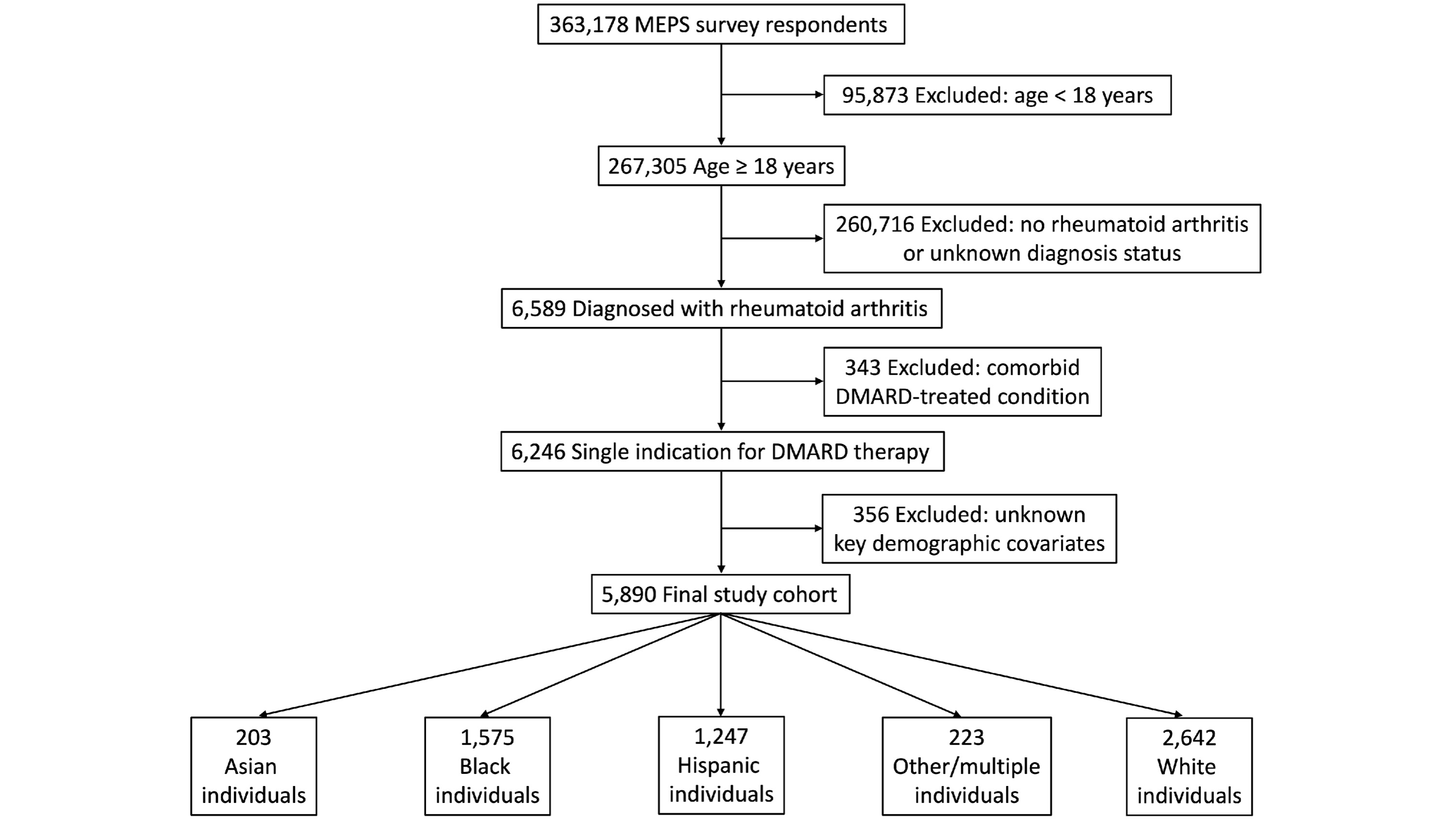
Methods: We developed a sample of RA patients aged 18 and older using the Medical Expenditure Panel Survey (MEPS) data from 2011 to 2021. Our primary outcomes were the utilization of any DMARD, csDMARDs, and bDMARDs. The main independent variable was self-reported race and ethnicity, categorized as Hispanic, Non-Hispanic Asian (Asian), Non-Hispanic Black (Black), Non-Hispanic ‘other race’ or ‘multiple races’ (Other/multiracial), and Non-Hispanic White (White).
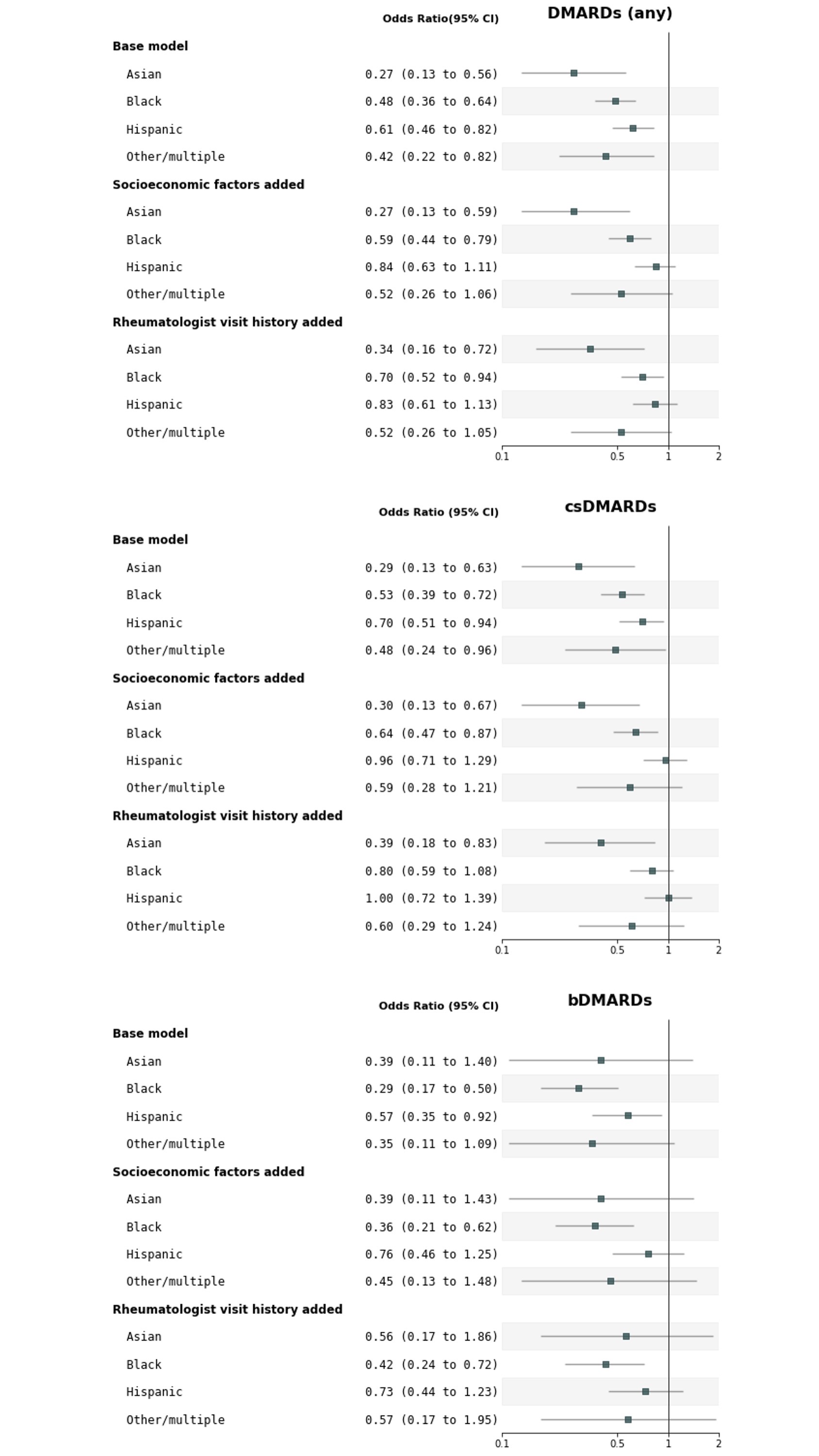
We used multivariable logistic regression to analyze racial and ethnic differences in DMARD utilization, adjusting for demographic and clinical characteristics, geographic region, year fixed effects; family income, education level, type of health insurance (socioeconomic factors); and history of rheumatology visits, utilizing a pharmacoequity conceptual framework. National estimates were produced using MEPS survey weights and cluster-robust standard errors.
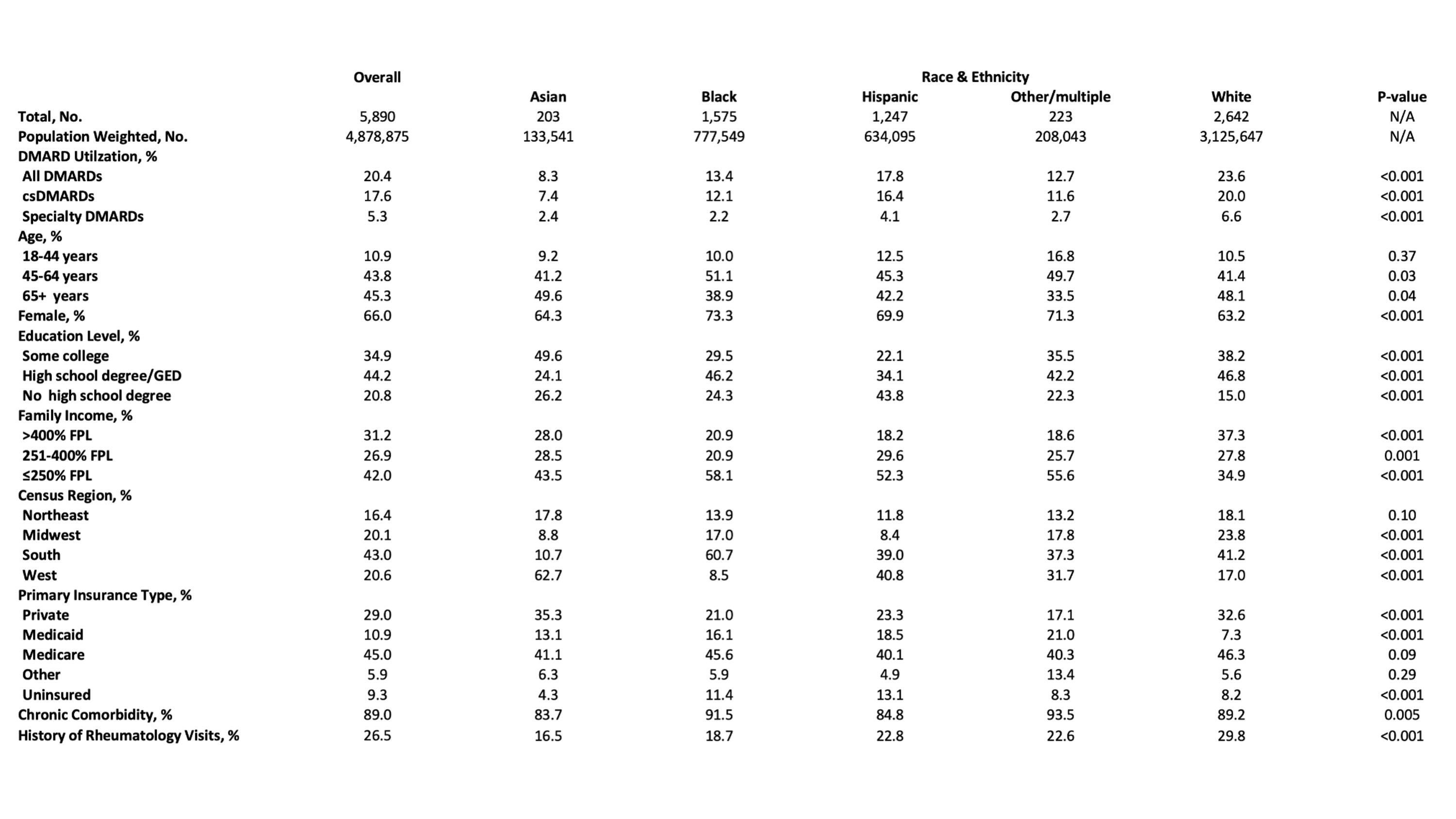
Results: We identified 5,890 adults diagnosed with RA, comprising 203 (2.7%) Asian, 1,575 (15.9%) Black, 1,247 (13.0%) Hispanic, 223 (4.3%) Other/multiracial, and 2,642 (64.1%) White patients (Figure 1). Minoritized patients had lower socioeconomic status and healthcare access compared to White patients (Table).
Unadjusted DMARD utilization rates were 20.4% for any DMARD, 17.6% for csDMARDs, and 5.3% for bDMARDs. White patients had the highest utilization rates, and the largest utilization gap was in bDMARDs (Table).
In the final adjusted model, Asian (aOR 0.34; 95% CI, 0.16-0.72) and Black (aOR 0.70; 95% CI, 0.52-0.94) patients had significantly lower odds of using any DMARD, driven by lower use of csDMARDs among Asian patients (aOR 0.39; 95% CI, 0.18-0.83) and bDMARDs among Black patients (aOR 0.42; 95% CI, 0.24-0.72). Initially significant lower odds for Hispanic and Other/multiracial patients were not significant after adjusting for socioeconomic factors (Figure 2).
Conclusion: In a national cohort of RA patients, we observed significantly lower DMARD utilization among Asian and Black patients compared to White patients. Specifically, Asian patients had lower csDMARD use, and Black patients had lower bDMARD utilization.
Our study has limitations. First, the cross-sectional nature of our data prevents us from establishing causal relationships. Second, we could not account for all bDMARDs and tsDMARDs. Third, the absence of RA disease severity data introduces potential confounding bias. Despite these limitations, our nationally representative data highlight significant racial disparities in DMARD utilization, particularly for costly bDMARDs, where access barriers are presumably higher.
To cite this abstract in AMA style:
Ara A, Chenoweth M, Kadiyala S, Essien U, Scannell C. Pharmacoequity of DMARDs Among Adults with Rheumatoid Arthritis in the U.S [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/pharmacoequity-of-dmards-among-adults-with-rheumatoid-arthritis-in-the-u-s/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pharmacoequity-of-dmards-among-adults-with-rheumatoid-arthritis-in-the-u-s/